Transcription of 1 AMERICAN SOCIETY OF ANESTHESIOLOGISTS PHYSICAL …
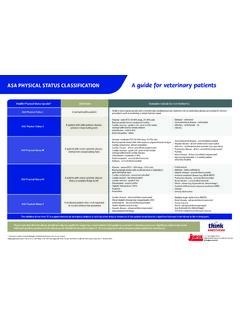
1 Copyright 2014 North Shore LIJ Health System Appendix 1 AMERICAN SOCIETY OF ANESTHESIOLOGISTS PHYSICAL STATUS CLASSIFICATION CLASS I No organic, physiological, biochemical or psychiatric disturbance. The pathologic process for which operation is to be performed is localized and is not a systemic disturbance. CLASS II Mild to moderate systemic disturbance caused either by the condition to be treated or by other pathophysiological processes. CLASS III Severe systemic disturbance or disease from whatever cause, even though it may not be possible to define the degree of disability with finality. CLASS IV Severe systemic disorder already life threatening, not always correctable by the procedure. CLASS V Moribund patient who has little chance of survival, but is submitted to the procedure in desperation. CLASS VI Organ donor. Copyright 2014 North Shore LIJ Health System Appendix 2 AIRWAY ASSESSMENT PROCEDURES FOR SEDATION Positive pressure ventilation, without endotracheal intubation, may be necessary if respiratory compromise develops during sedation / analgesia.
2 This may be more difficult in patients with atypical airway anatomy. Some airway abnormalities may increase the likelihood of airway obstruction during spontaneous ventilation. Factors that may be associated with difficulty in airway management are: HISTORY Previous problems with anesthesia or sedation Stridor, snoring or sleep apnea Dysmorphic facial features Tumor in airway Trauma to airway Radiation therapy to head, neck Advanced rheumatoid arthritis PHYSICAL EXAMINATION Habitus Significant obesity (especially involving the face, neck and thorax) Head and Neck Short neck, limited neck extension, decreased distance from the top of the mandible to the top of the thyroid cartilage (<3 cm in an adult); neck mass, cervical spine disease or trauma, tracheal deviation, decreased tissue compliance Mouth Small opening (<3 cm in an adult); edentulous or protruding incisors; loose or capped teeth; high arched palate; macroglossia; tonsillar hypertrophy.
3 Non visible uvula Jaw Micrognathia, retrognathia, trismus, significant malocclusion Copyright 2014 North Shore LIJ Health System Appendix 3 MALLAMPATI SCORE This scoring system was first introduced in 1985 in the Canadian Anesthesia SOCIETY Journal based on the work of Mallampati. Place the patient in a seated position and have them hold head in a neutral position with mouth open wide and the tongue fully extended. The paramedic should visualize one of the following classifications: Class I (easy) visualization of the soft palate, fauces, uvula, and both anterior and posterior pillars Class II visualization of the soft palate, fauces, and uvula Class III visualization of the soft palate and the base of the uvula Class IV (difficult) the soft palate is not visible at all Copyright 2014 North Shore LIJ Health System Appendix 4 FASTING PROTOCOL FOR SEDATION AND ANALGESIA FOR ELECTIVE PROCEDURES The following guidelines are intended for patients with normal airway and gastroesophageal anatomy.
4 Several factors are associated with delayed gastric emptying and/or increased risk of aspiration (see Appendix 5). When risk of aspiration is increased, a longer fasting interval is warranted and antacid prophylaxis or intubation may be indicated. 1 Chewing gum (chewed only, not swallowed) No delay 2 Clears, clear dissolving candy tic tacs, life savers (not chocolate) 2 Hours 3 Breast Milk 4 Hours 4 Formula, light carbohydrate meal (toast or crackers not containing fat, chocolate, protein or dairy products) 6 Hours 5 Fat, protein, non human milk 8 Hours *This includes milk, formula and breast milk (high fat content may delay gastric emptying). There are no data to establish whether a 6 8 hr fast is equivalent to an overnight fast before sedation / anesthesia. Copyright 2014 North Shore LIJ Health System Appendix 5 FACTORS ASSOCIATED WITH INCREASED RISK OF ASPIRATION Abnormal Airway Morbid Obesity Hiatus Hernia with Reflux Abnormal Autonomic Function Prior Gastric Surgery Pregnancy "Full Stomach" or Delayed Gastric Emptying Altered Mental State Spinal Cord Injury with Paraplegia or Quadriplegia Narcotics Pain Copyright 2014 North Shore LIJ Health System Appendix 6 DEPTH OF SEDATION CONTINUUM Approved by the ASA House of Delegates on October 13, 1999 and amended on October 27.
5 2004 Minimal Sedation Analgesia Moderate Sedation Deep Sedation General Anesthesia Responsiveness Normal response to verbal stimulation Purposeful response to verbal or tactile Purposeful response following repeated or painful stimulation Unarousable even with painful stimulus Airway Unaffected No intervention required Intervention may be required Intervention often required Spontaneous Ventilation Unaffected Adequate May be inadequate Frequently inadequate Cardiovascular Function Unaffected Usually maintained Usually maintained May be impaired Copyright 2014 North Shore LIJ Health System Appendix 7 MEDICATIONS FOR SEDATION The following are suggested doses. However, lower doses can have an unanticipated outcome. Any use of these medications for pre procedural sedation invokes the Sedation Protocol. MEDICATION DOSE COMMENTS SEDATIVES Midazolam (Versed) Adult: mg/kg IV Max 5 10 mg Peds: mg/kg IV mg/kg po Max: 20 mg po Additive depression with narcotics Lorazepam (Ativan) Adult: mg/kgMax: 4 mg Long acting Beware cumulative effect Diazepam (Valium) Adult: IVMax: 10 mg Pain on injection Half as potent as Versed Chloral hydrate Peds: 30 100 mg/kg po/prMax: 2 gm dose Must be given under supervisionANALGESICS Fentanyl (Sublimaze) Adult/Peds: 1 3 mcg/kg IVPotent synthetic Depressed CO2 response May outlast Narcan Morphine Adult/Peds: mg/kg IV Prototype narcotic Histamine release Long acting May outlast Narcan ANTAGONISTS Naloxone (Narcan) (for Narcotics) Adult: IVq 2 3 min to desired effect Peds: IV q 2 3 min Brief duration of action 30 45 minPotential for residual resedation Flumazenil (Romazicon) (for Benzodiazepines) Adult.
6 IV to desired effectAdult Max: 3 mg Peds Dose: Peds Max: May precipitate seizures Residual resedation Copyright 2014 North Shore LIJ Health System Appendix 7 continued DEEP SEDATION / ANESTHETICS These medications are commonly used to induce and/or maintain general anesthesia where loss of protective airway reflexes is anticipated. Therefore, these medications are not suitable for conscious sedation/analgesia. Their use is restricted to specifically credentialed physician practitioners. DEEP SEDATION / ANESTHETICS MEDICATION DOSE COMMENTS Propofol (Diprivan) Adult: 1mg/kg followed by q 3 5 minutes as needed Peds: 1mg/kg followed by every 3 5 minutes as needed Short acting hypnotic. Respiratory depressant. Antiemetic. Onset within 30 seconds. IV lasts 3 10 minutes depending on dose No analgesic properties Vasodilator and Negative Inotrope May need to reduce dose in elderly Etomidate (Amidate) Adult: IV push over 30 60 sec.
7 Then q 3 5 min. Peds: Irritating at injection site. Lasts: (Dose dependent) 2 3 min 4 10 min Ketamine Adults: 1 to 2mg/kgIV over 1 2 min. Then q 5 10 min Peds: Onset within 30 seconds IV lasts 5 to10 minutes. Maximum concentration for IV push 50 mg/ml Recovery 1 2 hours Copyright 2014 North Shore LIJ Health System Appendix 8 RELEVANT JOINT COMMISSION and ASA STANDARDS 1. To review the relevant Joint Commission Standards please see 2009 Hospital Accreditation Standards: to , , 2. To review the relevant AMERICAN SOCIETY of Anesthesia Standards see Practice Guidelines for Sedation and Analgesia by Non ANESTHESIOLOGISTS in Anesthesiology 2002; 96:1004 17 Copyright 2014 North Shore LIJ Health System Appendix 9 Forms: 1. Suggested Pre Procedure Assessment Record 2. Required Sedation Procedure Record NORTH SHORE-LIJ HEALTH SYSTEM SEDATION RECORD Copyright 2014 North Shore LIJ Health System Appendix 10 ALDRETE SCORE 0 2 Activity: Able to Move on Command.
8 2 Impaired Movement .. 1 Not Moving .. 0 Respiration: Able to Breathe Freely .. 2 Dyspnea or Limited Breathing .. 1 Apneic .. 0 Consciousness: Fully Awake .. 2 Arousable on Calling .. 1 Not Responding .. 0 Circulation: Within Normal BP/Pulse Range .. 2 Impaired Circulation .. 1 Unstable .. 0 Oxygen Saturation (Pulse Oximetry): >92% on Room 2 Needs Supplemental Oxygen to Maintain Saturation >90% .. 1 <90% even with Supplemental Oxygen .. 0 Copyright 2014 North Shore LIJ Health System Appendix 11 NORTH SHORE LIJ POST ANESTHESIA SCORE 1. Activity 2 = Not Applicable 2 = Able to move 4 extremities voluntarily 1 = Able to move 2 extremities voluntarily 0 = Unable to move extremities voluntarily 2. Respiratory 2 = Able to breathe and cough freely 1 = Dyspnea, limited breathing or tachypnea 0 = Apnea or mechanical ventilator 3. Blood Pressure 2 = BP within 20% of preanesthetic level 1 = BP within 20 49% of preanesthetic level 0 = BP within 50% of preanesthetic level 4.
9 Level of Consciousness 2 = Fully awake 1 = Arousable on calling 0 = Not responding 5. O2 Saturation 2 = Able to maintain O2sat >92% on room air 1 = Needs O2 therapy to maintain O2sat >90% 0 = O2 saturation <90% even with O2 supplement 6. Dressing 2 = Not applicable 2 = Dry and clean 1 = Wet but marked and not increasing 0 = Growing area of wetness 7. Pain 2 = Pain free 1 = Mild pain 0 = Severe pain 8. Ambulation / Mobility 2 = Not applicable 2 = Return to prior level of activity 1 = Dizziness when erect 0 = Dizziness when supine 9. Fasting / Feeding 2 = Not applicable 2 = Able to drink fluids 1 = Nauseated 0 = Nausea and vomiting 10. Urine Output 2 = Not applicable 2 = Has voided 1 = Unable to void but comfortable 0 = Unable to void and uncomfortable