Transcription of A review of self-medication in physicians and medical students
1 Occupational review of self - medication in physicians andmedical studentsA. J. Montgomery1, C. Bradley2, A. Rochfort3and E. Panagopoulou41 Department of Education and Social Policy, University of Macedonia, Egnatia Street 156, Thessaloniki 54006, Greece,2 Department of General Practice, Western Gateway Building, University College Cork, Ireland,3 The Irish College of GeneralPractitioners, 4/5 Lincoln Place, Dublin, Ireland,4 medical School, Aristotle University Thessaloniki, University campus,Thessaloniki 55131, to: A. J. Montgomery, Department of Education and Social Policy, University of Macedonia, Egnatia Street 156,Thessaloniki 54006, Greece. Tel: +30 2310891308; e-mail: is a culture within medicine that doctors do not expect themselves or their colleagues to be , the associated complexities of self -diagnosis, self -referral and self -treatment among physiciansare significant and may have repercussions for both their own health and, by implication, for thequality of care delivered to collate what is known about the self -treatment behaviour of physicians and medical following databases were searched: PubMed, PsychInfo, EBSCO, Medline, BioMed central andScience Direct.
2 Inclusion criteria specified research assessing self -treatment and self -medicating ofprescription drugs among physicians and/or medical students . Only peer-reviewed English languageempirical studies published between 1990 and 2009 were studies were identified that fitted the inclusion criteria. self -treatment and self -medicating was found to be a significant issue for both physicians and medical students . In 76%of studies, reported self -treatment was>50% (range: 12 99%). Overall, only one of two respondentswas registered with a general practitioner or primary care physician (mean556%, range521 96).Deeper analysis of studies revealed that physicians believed it was appropriate to self -treat both acuteand chronic conditions and that informal care paths were common within the medical is strongly embedded within the culture of both physicians and medical students as anaccepted way to enhance/buffer work performance.
3 The authors believe that these complex self -directed care behaviours could be regarded as an occupational hazard for the medical wordsOccupational hazard; fitness for work; occupational; occupational fitness; occupational medicine ed-ucation; workplace; workplace hazards; it comes to their own health, doctors may behaveirrationally and paradoxically. The medical profession ex-pect patients to seek appropriate medical help when theyencounter significant problems with their health and yetdoctors do not behave in this way when it comes to theirown health [1]. self -prescription by physicians and otherforms of inappropriate self -treatment by both physiciansand medical students represent serious issues for bothpatients and physicians .
4 For the physician , there is the ob-vious threat to their health of inappropriate subjective ordelayed objective treatment [2]. For the patient, a physi-cian whose health is impaired is at risk of not being able todeliver care of the expected quality [3,4]. self -treatmentrepresents a threat to professionalism within medicineand has the potential to erode the public s trust in the pro-fession [5]. If doctors cannot be trusted to acknowledgeand seek appropriate care as a patient for their own phys-ical and mental health can they be trusted to care appro-priately for their patients? The aim of this systematicreview is to collate what is known about the self -treatmentbehaviour of physicians and medical following keywords were used in the electronicdatabases: physician use of health care; health status; doc-tors personal health care choices, doctors as patients, The Author 2011.
5 Published by Oxford University Press on behalf of the Society of Occupational rights reserved. For Permissions, please email: Occupational Medicine Advance Access published July 4, 2011 by guest on July 11, from self -treatment, self - medication , self -prescription, doctors illnessbehaviour,doctors health,healthcareseekingbehav-iour, psychology and attitudes to health. Searched data-bases included the following: PubMed, PsychInfo,EBSCO, Medline, BioMed central and Science systematic review was conducted in distinctphases and adhered to the guidelines of Petticrew andRoberts [6].The Searching phase involved the systematic identi-fication of potentially relevant studies. In the second Screening phase , predetermined inclusion and exclu-sion criteria were applied to identify the appropriatestudies.
6 In the third Data-extraction phase , there wasan in-depth examination of studies, meeting the inclusionand exclusion criteria, to assess the quality of the studyand extract the evidence that is needed. In the fourth Synthesis phase , the authors developed a frameworkfor analysing the selected the present study, the inclusion and exclusion crite-ria were derived from (i) an examination of a sample oftarget papers in the field, (ii) discussion and reviewsamong the authors as to what samples and issue were rel-evant to the focus of the study and finally (iii) the devel-opment of a specified checklist to describe the criteria included were required to be: (i) written inEnglish; (ii) conducted between 1990 and 2009;(iii) drawn from both published and/or unpublished re-search; (iv) focused on the self -treatment behaviour ofphysicians and medical students .
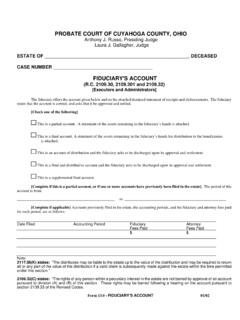
7 (v) reported quantita-tive statistics that provided information on sample sizes,response rates methodology used and statistical that were excluded from the search were(i) not written in English; (ii) conducted before 1990;(iii) not based on empirical research; (iv) based on a singleperson s opinion and (v) concerned with illegal substanceabuse among physicians and medical 1 [7 33] presents the results of the review . In total,27 studies (see Figure 1) were located that fitted theinclusion criteria. The majority (21/27) of studies werecross-sectional and relied on self -report. The aggregatesample size of the 27 studies was 28 628 (range554 5426); and the average response rate was 66%.In 76% studies, reported self -treatment (range: 12 99%).
8 Overall, only one of two respondentswas registered with general practitioner (GP) or primarycare physician (mean556%, range521 96). In the 23studies providing information on self -prescription, themean number of physicians reporting self -prescriptionwas 61% with an SD of 25% and a range of 9 99%.The relatively small number of studies identifiedallowed for a more qualitative analysis of the reviewedresearch. Therefore, the first and fourth authors con-ducted a content analysis of the research literature usingthe technique of interpretative phenomenological analysis(IPA). The aim of IPA is to explore in detail the topicunder investigation (individual level) and to facilitatethe identification of shared categories (group level).
9 The steps, as recommended by Smithet al.[34], areas follows: (i) the script is read through, with initialthoughts and possible codes/themes noted down; (ii) onceclusters of themes have been produced for the first inter-view/text, the coding process is repeated for each paper inturn; (iii) clusters of themes are gathered together to iden-tify general themes; (iv) once these broader themes havebeen identified, researchers go back to the text to verifythat there was evidence for these themes; (v) these broad-er themes are then examined to see whether they can begrouped together in a meaningful way; (vi) codes arerechecked and assigned numerical codes for ease ofanalysis and grouping and (viii) it is then possible to cap-ture emergent themes.
10 This process is continued in an it-erative fashion until the researcher reaches a point key themes were identified as driving the inappro-priate self -treatment behaviours of physicians andmedical students : (i) avoiding the role of patient; (ii)acceptance of self -treatment as the norm (for variousreasons, the alternative, going to another doctor, is lessacceptable and less attractive); (iii) work performanceor pressure to remain at work and (iv) protecting or keep-ing things within the control of the individual professionalor a small number of chosen colleagues there is a strongincentive to retain privacy of health and medical students find it challenging to bea patient as a result of their medical training and attitudesand are often regarded as reluctant or even difficultpatients by health professionals who treat them.