Transcription of ACOG PRACTICE BULLETIN - Preeclampsia
1 INTERIM UPDATEACOG PRACTICE BULLETINC linical Management Guidelines for Obstetrician GynecologistsNUMBER222(Replaces PRACTICE BULLETIN No. 202, December 2018)Committee on PRACTICE Bulletins PRACTICE BULLETIN was developed by the American College of Obstetricians andGynecologists Committee on PRACTICE Bulletins Obstetrics in collaboration with Jimmy Espinoza, MD, MSc; Alex Vidaeff, MD,MPH; Christian M. Pettker, MD; and Hyagriv Simhan, UPDATE: The content of this PRACTICE BULLETIN has been updated as highlighted (or removed as necessary) toinclude limited, focused editorial corrections to platelet counts, diagnostic criteria for Preeclampsia (Box 2), and pre-eclampsia with severe features (Box 3).Gestational Hypertension andPreeclampsiaHypertensive disorders of pregnancy constitute one of the leading causes of maternal and perinatal mortalityworldwide.
2 It has been estimated that Preeclampsia complicates 2 8% of pregnancies globally (1). In LatinAmerica and the Caribbean, hypertensive disorders are responsible for almost 26% of maternal deaths,whereas in Africa and Asia they contribute to 9% of deaths. Although maternal mortality is much lower inhigh-income countries than in developing countries, 16% of maternal deaths can be attributed to hypertensivedisorders (1, 2). In the United States, the rate of Preeclampsia increased by 25% between 1987 and 2004 (3).Moreover, in comparison with women giving birth in 1980, those giving birth in 2003 were at increasedrisk of severe Preeclampsia (4). This complication is costly: one study reported that in 2012 in the United States,the estimated cost of Preeclampsia within the first12 months of delivery was $ billion ($ billion forwomen and $ billion for infants), which was disproportionately borne by premature births (5).
3 ThisPractice BULLETIN will provide guidelines for the diagnosis and management of gestational hypertension FactorsA variety of risk factors have been associated withincreased probability of Preeclampsia (Box 1) (6 12). Nonetheless, it is important to remember thatmost cases of Preeclampsia occur in healthy nullipa-rous women with no obvious risk factors. Althoughthe precise role of genetic environmental inter-actions on the risk and incidence of Preeclampsia isunclear, emerging data suggest the tendency todevelop Preeclampsia may have some genetic com-ponent (13 16).Definitions and Diagnostic Criteria forHypertensive Disorders of PregnancyPreeclampsia (With and WithoutSevere Features) Preeclampsia is a disorder of pregnancy associated withnew-onset hypertension, which occurs most often after 20weeks of gestation and frequently near term.
4 Althoughoften accompanied by new-onset proteinuria, hypertensionand other signs or symptoms of Preeclampsia may presentin some women in the absence of proteinuria (17). Reli-ance on maternal symptoms may be occasionally problem-atic in clinical PRACTICE . Right upper quadrant or epigastricVOL. 135, NO. 6, JUNE 2020 OBSTETRICS & GYNECOLOGYe237 2020 by the American College of Obstetriciansand Gynecologists. Published by Wolters Kluwer Health, reproduction of this article is is thought to be due to periportal and focal parenchy-mal necrosis, hepatic cell edema, or Glisson scapsuledistension, or a combination. However, there is not alwaysa good correlation between the hepatic histopathology andlaboratory abnormalities (18). Similarly, studies havefound that using headache as a diagnostic criterion forpreeclampsia with severe features is unreliable and non-specific.
5 Thus, an astute and circumspect diagnosticapproach is required when other corroborating signs andsymptoms indicative of severe Preeclampsia are missing(19, 20). Of note, in the setting of a clinical presentationsimilar to Preeclampsia , but at gestational ages earlier than20 weeks, alternative diagnoses should to be considered,including but not limited to thrombotic thrombocytopenicpurpura, hemolytic uremic syndrome, molar pregnancy,renal disease or autoimmune hypertension and proteinuria are consid-ered to be the classical criteria to diagnose Preeclampsia ,other criteria are also important. In this context, it isrecommended that women with gestational hypertensionin the absence of proteinuria are diagnosed with pre-eclampsia if they present with any of the followingsevere features: thrombocytopenia (platelet count lessthan 100,0003109/L); impaired liver function as indi-cated by abnormally elevated blood concentrations ofliver enzymes (to twice the upper limit of normal con-centration); severe persistent right upper quadrant or epi-gastric pain and not accounted for by alternativediagnoses; renal insufficiency (serum creatinine concen-tration greater than mg/dL or a doubling of the serumcreatinine concentration in the absence of other renaldisease); pulmonary edema.
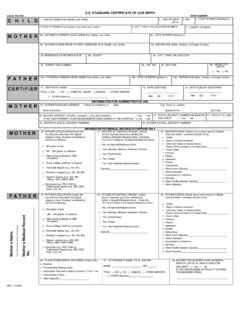
6 Or new-onset headache unre-sponsive to acetaminophen and not accounted for byalternative diagnoses or visual disturbances (Box 2).Ges-tational hypertensionis defined as a systolic blood pres-sure of 140 mm Hg or more or a diastolic blood pressureof 90 mm Hg or more, or both, on two occasions at least4 hours apart after 20 weeks of gestation in a womanwith a previously normal blood pressure (21). Womenwith gestational hypertension with severe range bloodpressures (a systolic blood pressure of 160 mm Hg orhigher, or diastolic blood pressure of 110 mm Hg orhigher) should be diagnosed with Preeclampsia withsevere features. These severe ranges of blood pressureor any of the severe features listed in Box 3 increasethe risk of morbidity and mortality (22).Box 1. Risk Factors for PreeclampsiaNulliparityMultifetal gestationsPreeclampsia in a previous pregnancyChronic hypertensionPregestational diabetesGestational diabetesThrombophiliaSystemic lupus erythematosusPrepregnancy body mass index greater than 30 Antiphospholipid antibody syndromeMaternal age 35 years or olderKidney diseaseAssisted reproductive technologyObstructive sleep apneaBox 2.
7 Diagnostic Criteria forPreeclampsiaBlood pressurecSystolic blood pressure of 140 mm Hg or more ordiastolic blood pressure of 90 mm Hg or more ontwo occasions at least 4 hours apart after 20weeks of gestation in a woman with a previouslynormal blood pressurecSystolic blood pressure of 160 mm Hg or more ordiastolic blood pressure of 110 mm Hg or more.(Severe hypertension can be confirmed withina short interval (minutes) to facilitate timelyantihypertensive therapy).andProteinuriac300 mg or more per 24 hour urine collection (orthis amount extrapolated from a timed collection)orcProtein/creatinine ratio of or more orcDipstick reading of 2+ (used only if other quan-titative methods not available)Or in the absence of proteinuria, new-onset hyper-tension with the new onset of any of the following:cThrombocytopenia: Platelet count less than100,0003109/LcRenal insufficiency: Serum creatinine concen-trations greater than mg/dL or a doubling ofthe serum creatinine concentration in theabsence of other renal diseasecImpaired liver function.
8 Elevated blood concen-trations of liver transaminases to twice normalconcentrationcPulmonary edemacNew-onset headache unresponsive to medicationand not accounted for by alternative diagnoses orvisual symptomse238 PRACTICE BulletinGestational Hypertension and PreeclampsiaOBSTETRICS & GYNECOLOGY 2020 by the American College of Obstetriciansand Gynecologists. Published by Wolters Kluwer Health, reproduction of this article is pregnancy is defined as 300 mg/dL of protein or more in a 24-hour urine collection (21,23) or a protein -to-creatinine ratio of or more (24).When quantitative methods are not available or rapiddecisions are required, a urine protein dipstick readingcan be substituted. However, dipstick urinalysis has highfalse positive and false negative test results. A test resultof 1+ proteinuria is false positive in 71% of casescompared with the 300 mg cutoff on 24-hour urine col-lection, and even 3+ proteinuria test results may be false positive in 7% of cases.
9 Using the same 24-hour urinecollection standard, the false negative rate for dipstickurinalysis is 9% (25). If urinalysis is the only availablemeans of assessing proteinuria then overall accuracy isbetter using 2+ as the discriminant value (25, 26).Gestational HypertensionGestational hypertensionis defined as a systolic bloodpressure 140 mm Hg or more or a diastolic blood pres-sure of 90 mm Hg or more, or both, on two occasions atleast 4 hours apart after 20 weeks of gestation, ina woman with a previously normal blood pressure (21).Gestational hypertension is considered severe when thesystolic level reaches 160 mm Hg or the diastolic levelreaches 110 mm Hg, or both. On occasion, especiallywhen faced with severe hypertension, the diagnosismay need to be confirmed within a shorter interval (mi-nutes) than 4 hours to facilitate timely antihypertensivetherapy (27).
10 Gestational hypertension occurs whenhypertension without proteinuria or severe features de-velops after 20 weeks of gestation and blood pressurelevels return to normal in the postpartum period (21). Itappears that this diagnosis is more of an exercise ofnomenclature than a pragmatic one because the manage-ment of gestational hypertension and that of preeclamp-sia without severe features is similar in many aspects, andboth require enhanced surveillance. Outcomes in womenwith gestational hypertension usually are good, but thenotion that gestational hypertension is intrinsically lessconcerning than Preeclampsia is incorrect. Gestationalhypertension is associated with adverse pregnancy out-comes (17) and may not represent a separate entity frompreeclampsia (28). Up to 50% of women with gestationalhypertension will eventually develop proteinuria or otherend-organ dysfunction consistent with the diagnosis ofpreeclampsia, and this progression is more likely whenthe hypertension is diagnosed before 32 weeks of gesta-tion (29, 30).