Transcription of Arteriovenous Malformation of the Stomach: A Rare Cause of ...
1 142 Med J Malaysia Vol 66 No 2 June 2011 SUMMARYH aemorrhage arising from gastric arteriovenousmalformation (AVM) is rare and normally occurs in theelderly. Bleeding gastric AVM presenting in the younger agegroup is even rarer. We report a case of a 14 year old boywho presented with recurrent episodes of subsequently underwent a proximal gastrectomy and thehistological examination confirmed a gastric AVM. Afterreviewing the literature we believe this is the youngest everreported case of bleeding gastric AVM reported in WORDS: Arteriovenous Malformation , upper gastrointestinal bleeding,stomachINTRODUCTIONH aemorrhage from upper gastrointestinal tract (GIT) iscommonly due to bleeding peptic ulcer disease, oesophagealvarices and Mallory-Weiss tear. On the other hand, bleedingfrom gastric Arteriovenous Malformation (AVM) is anextremely uncommon occurrence accounting for only 1 - 2%of upper GI haemorrhage cases1.
2 In addition, a slow,intermittent bleed makes the diagnosis difficult andchallenging. Most reports postulate an acquired degenerativeaetiology making the commonest age of presentation to be inthe 60s to80s2. Thus far, the youngest patient reported withgastric AVM was 38 years of age. We present a case of chronic,intermittent upper GIT bleed in a young teenager who waseventually diagnosed to have AVM at the fundus of REPORTA 14-year old boy was referred from another hospital forfurther management after he presented with 3 monthshistory of intermittent fresh haematemesis associated withleft hypochondrium pain. The bleeding was minimal (1 to2ml) and intermittent every 2 to 3 weeks. He was admitted afew times to the previous hospital during which his bloodpressure and pulse remained stable while his haemoglobinnever dropped below 12g/dL. He was otherwise healthy withno family history of bleeding investigations had been performed during previoushospital admissions which includedoesophagogastroduodenoscopy (OGDS), bronchoscopy,fibreoptic nasophayngolaryngoscopy, ComputedTomography (CT) of abdomen and barium meal and follow-through.
3 All results were normal. He was then transferred toour hospital. During the first hospital admission here, anOGDS done during the acute bleeding episode revealedsubmucosal haemorrhages at the gastric fundus with bloodclots and no active bleeding noted. He was observed for 3days and later discharged after no further bleeding he was readmitted 2 weeks later as hedeveloped another episode of haematemesis and repeatOGDS revealed focal areas of inflammation with focalumbilicated ulcer or fissure at fundus of the stomach withcontact bleeding. The lesion was coagulated with argon (APC)but he continued to have haematemesis a few days laterduring the same admisssion. With the inconclusiveendoscopic studies, we decided to proceed with coeliacangiographic study which did not show any abnormality. Atthis point, differential diagnoses of gastrointestinal stromaltumour (GIST), leiomyoma and vascular Malformation wereentertained.
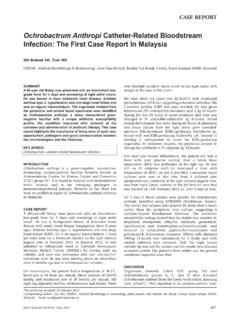
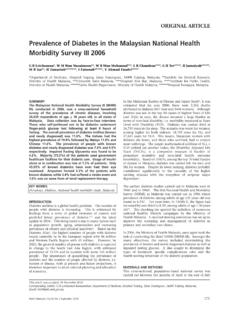
4 An endoscopic ultrasonography (EUS) showed a6-mm submucosal lesion at the fundus of the stomach (Figure1). With a preoperative diagnosis of GIST, a laparoscopicwedge resection of the lesion was laparoscopy, there was difficulty in identifying thelesion even after adequate mobilization of the gastric was converted to an upper midline inspection and palpation of the stomach was anterior gastrostomy was performed but no abnormalitieswere seen from within. A proximal gastrectomy withpyloroplasty was decided upon based on the pre operativeEUS , the specimen showed a few areas of dark brownmucosa on the marked anterior wall with no obvious mass orulcer noted. Microscopically, there were extensive mucosaland submucosal haemorrhages with increased number ofdilated and congested blood vessel consistent with AVM ofthe stomach (Figure 2). The patient recovered well from and vascular ectasia are the subsets ofarteriovenous Malformation (AVM) which constitute thepresence of dilated and tortuous vessels2.
5 AVM of thegastrointestinal tract have been found to be the single mostArteriovenous Malformation of the stomach : A Rare Causeof Upper Gastrointestinal BleedingN H M Latar, MBBS, MS, K S Phang, MBBS(Mal), DCP(Lond), J A Yaakub, MBChB(Cairo), MS( ) (UKM),FRCS(Edin), R Muhammad, BSc. MB. ChB(Glasg), MS(UKM), FRCS(Glasg), AM(Mal)Universiti Kebangsaan Malaysia Medical Centre, Department of Surgery, Jalan Yaakub Latiff, Cheras, 56000 Kuala Lumpur,MalaysiaCASE REPORTThis article was accepted: 16 May 2011 Corresponding Author: Nani Harlina - Md Latar, Universiti Kebangsaan Malaysia Medical Centre, Department of Surgery, Jalan Yaakub Latiff, Cheras,56000 Kuala Lumpur Malaysia Email: Malformation of the stomach : A Rare Cause of Upper Gastrointestinal BleedingMed J Malaysia Vol 66 No 2 June 2011143common Cause of chronic and massive haemorrhage whenconventional diagnostic tools failed to reveal the cause2. Itaccounts for only 1 - 2% of upper GI haemorrhage1.
6 Commonsite for bleeding AVM is the caecum and ascending colon( ), while bleeding from other sites being quite rare;jejunum ( ), ileum ( ) and stomach ( )3. In thepresent case, we had difficulty making the diagnosis due tothe small amount of bleeding and the rare site of Cause of GI AVM is unclear but many had attributed it tothe degenerative changes on the wall of the bowel3. Thismakes the disease to be more prevalent among the 60s to 80sage group. AVM occuring at sites other than the colon wasbelieved to be congenital in origin, but the youngest patientreported so far in the English literature is 38 years old. Thus,our patient is the youngest patient currently diagnosed withbleeding gastric GI endoscopy remains the first diagnosticinvestigation for patients with upper GIT bleeding. Locatinga gastric AVM can be successfully made by OGDS, but its roleis limited in an actively bleeding lesion4. Macroscopically itmay appear as flat or nodular bright red lesion and sometimesappear in telengiactatic form.
7 Endoscopic ultrasound (EUS)has been proven to accurately detect submucosal EUS, AVMs appear as hypoechoeic structure insubmucosal layer and can be easily differentiated fromnonvascular structure using an echoendoscope using colourDoppler. However it might fail to disclose the diagnosis in22% of patients3. As in our case we did not proceed withcolour Doppler study thus the vascular nature of the lesionwas not confirmed5. Accurate bleeding site is the most important factor indetermining the appropriate management of patients withAVMs of the GIT. Moore et al had studied 17 patients withbleeding AVM and found out that most bleeding site can beaccurately determined preoperatively by selectiveangiographic studies3. It has a diagnostic accuracy of 50 to75%, but this approaches 90% if the procedure is performedwhile the patient is actively bleeding.
8 However the coeliacangiography in our patient failed to reveal any abnormalitiesand this was probably due to the intermittent and smallamount of bleeding from the CT and Magnetic Resonance Imaging (arteriography)MRI (A) had their established role in diagnosis andmanagement of cerebral AVM, their role in evaluating GIAVM is still not of much value. CT in our case was performedto look for bowel related masses as the Cause of bleeding. Close long term follow up is important in patient with AVMas post operative bleeding ranges from 5% to 37%4. This issecondary to incomplete initial resection and/ormetachronous AVMs which have been reported in 11% ofcases4. Our patient had been followed up for 3 months withno recurrence of summary, gastric AVM should be considered as a rare causeof upper GI bleed in cases where no other abnormalities canbe detected. Diagnosis however can be extremely difficult asthey may present with a small intermittent bleed asillustrated in our patient.
9 Our patient was the youngest everreported with such a problem in the English Huang C, Lichtenstein D. Nonvariceal upper gastrointestinal Clin N Am 2003; 32(4): Gordon F, Watkinson A, Hodgson H. Vascular malformations of thegastrointestinal tract. Best Pract & Research Clin Gastroenterology 2001;15(1): Moore J, Thompson N, Appelman H et al. Arteriovenous malformations ofthe gastrointestinal tract. Arch Surg 1976; 111: Kono K, Sekikawa T, Iino T et al. A case of Arteriovenous Malformation inthe submucosal layer of the stomach . J Gastroenterology 1994; 29: 1:Endoscopic ultrasonography showing submucosal lesion(arrow).Fig. 2:Section shows oedematous submucosa with abnormal,dilated and congested blood vessels within.