Transcription of Biochemical and Haematological Targets: Haemoglobin …
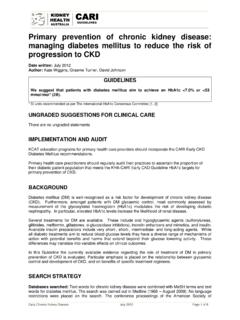
1 The KHA-CARI Guidelines Caring for Australasians with Renal Impairment Biochemical and Haematological targets (October 2011) Page 1 Biochemical and Haematological targets : Haemoglobin Levels in Patients Using Erthyropoiesis Stimulating Agents Date written: May 2011 Final submission: October 2011 Author: Lawrence McMahon, Rob MacGinley GUIDELINES a. We recommend against Haemoglobin (Hb) targets above 130 g/L due to the strong association with increased morbidity and mortality in chronic kidney disease (CKD) (1A)*. b. For many anaemic patients with CKD we suggest a Hb target of between 100 and 115 g/L, balancing risks and benefits for each patient treated, in order to alleviate symptoms and reduce the risk of blood transfusion (2A)*. c. We suggest that in dialysis patients with anaemia due to CKD, an erythropoiesis stimulating agent (ESA) can be used to prevent the Hb falling below 95 g/L in order to avoid the need for blood transfusion (2B)* and to improve quality of life (2D)*.
2 D. We suggest that ESAs are indicated for the partial correction of the anaemia of CKD in patients who are symptomatic or who may otherwise require blood transfusion (2A)*. UNGRADED SUGGESTIONS FOR CLINICAL CARE Treatment with Erythropoiesis Stimulating Agents (ESAs) Prior to the commencement of administration of ESAs, appropriate iron indices should be ensured. In addition, efforts should be made to control hyperparathyroidism, aluminium accumulation and/or significant systemic inflammation. Blood pressure levels should be controlled according to standard guidelines. For any individual patient who may require ESA therapy, the potential benefits must be balanced with the clinical risks. General Points Readers should refer to the PI (Product Information) brochures for the various ESAs currently available in Australia and/or New Zealand for information concerning mode and frequency of administration, and for side effects.
3 All agents (apart from the newly listed epoetin lamba) currently have approval for both intravenous and subcutaneous administration. Increments in dosage should be considered if there is an inadequate increase in Haemoglobin concentration (10 g/L) after a 4-week period. The Haemoglobin concentration is usually checked at least monthly initially, and/or 1 month after a change in ESA dosage. Dosages in excess of 200 U/kg per week (or equivalent) in the setting of significant systemic inflammation are unlikely to elevate Haemoglobin concentrations further. In the absence of inflammation, The KHA-CARI Guidelines Caring for Australasians with Renal Impairment Biochemical and Haematological targets (October 2011) Page 2 assessment of Vitamin B12 and folate stores and/or exclusion of occult bleeding may be required.
4 On average, after initiation of treatment, the rise in Haemoglobin concentrations should not exceed 10 g/L per 2 week period). The Haemoglobin concentration should be checked at least every month initially and iron stores at least every 3 months. There are no studies that have ascertained whether CKD patients (including dialysis), who are ESA-naive, and who have a normal or high Haemoglobin concentration have an increased risk of morbidity or mortality. Accordingly, these guidelines are specific for ESA-dependent patients with CKD. IMPLEMENTATION AND AUDIT 1. The percentage of patients on ESAs reaching the target Haemoglobin concentration should be calculated against the total population treated with ESA s. 2. The number of patients not requiring ESA should be monitored, and patients followed for access thrombosis and mortality. 3. The percentage of patients requiring more than 20,000 units of epoetin alfa or epoetin beta or 100 g of darbepoetin per week should be assessed and quantified against inflammatory markers.
5 4. The percentage of patients exceeding physiological Haemoglobin concentrations on ESAs (both pre- and post-dialysis in haemodialysis patients) should be calculated. 5. The percentage of patients requiring cessation or reduction in epoetin dosage because of uncontrolled hypertension or an excessively rapid rise in Haemoglobin levels (>10 g per 2 weeks) should be assessed. BACKGROUND Anaemia is an almost universal accompaniment of CKD. Several of the co-morbidities associated with kidney failure have been primarily attributed to anaemia, including the development of left ventricular dysfunction, cardiac failure, reduced exercise capacity and reduced quality of life. Prior to the synthesis of epoetin, transfusion dependence was characterised by blood-borne infection, iron overload and sensitisation to HLA antigens, which limited transplantation opportunities.
6 With the availability of epoetin analogues (epoetin alfa, epoetin beta, darbepoetin alfa and others), collectively known as erythropoiesis-stimulating agents (ESAs), clinicians, patients and funders of health care require information about their effectiveness as well as the clinical consequences and economic impact of an increase in Haemoglobin . These guidelines were developed to present and integrate the available evidence. Target Haemoglobin Observational studies have uniformly demonstrated that people with innate higher Haemoglobin concentrations enjoy better outcomes, including fewer hospitalizations and longer survival. Randomized controlled trials of patients receiving an ESA, on the other hand, show that the risk of stroke, hypertension and vascular thrombosis are greater when the target Hb is 130g/L. A meta analysis of all RCTs shows a strong trend in all-cause and cardiovascular mortality [1].
7 This effect could be related to the rate of increase in Haemoglobin concentration, as well as to an overshoot of the target. Another possibility is that adverse cardiovascular events are not related to Haemoglobin concentrations at all but are instead due to pleomorphic effects of ESAs through trophic effects on vascular endothelial or smooth muscle cells, particularly if precipitated by exposure to a higher The KHA-CARI Guidelines Caring for Australasians with Renal Impairment Biochemical and Haematological targets (October 2011) Page 3 ESA dose ( iron deficiency). An association between high-dose ESA use and both accelerated tumour progression and shortened survival has been observed in patients with active malignancy. Hence, as will be evident from analysis of the evidence below, it is now necessary for protagonists of higher Haemoglobin targets to justify their claim in specific individuals.
8 There are, for instance, no data to suggest that the minority of CKD patients who maintain their Haemoglobin concentrations above the proposed target without the need for ESA should have their levels reduced by venesection; similarly, the appropriate Haemoglobin target for patients with chronic airflow obstruction, for patients on peritoneal dialysis, the elderly, the very young, and those with sickle cell disease, thalassaemia or concurrent cyanotic cardiac disease may require specific targets yet to be determined. Other issues remain and/or require further clarification. For haemodialysis patients, for instance, Haemoglobin concentration is conventionally measured before dialysis. There are fears that excessive ultrafiltration may produce dangerously high haematocrit levels with associated intravascular red cell sludging or thrombosis if the baseline haematocrit is kept at more than 39% [2-4].
9 Changes in haematocrit from the start to end of dialysis can vary by as much as 3-6% [5, 6] depending on the volume of ultrafiltration and the timing of the post-dialysis sample. It would seem prudent to also measure the post-dialysis Haemoglobin concentration in patients when the pre-dialysis level is above 130 g/L to ensure that haemoconcentration during dialysis does not exceed physiological limits. Quality of Life Investigation of ESAs and quality of life is complicated by the classification of patients, research design, the choice of instruments used to measure quality of life, and the definition of clinically meaningful improvement in quality-of life domains. There has been a need to identify clinical benefits related to raising the Haemoglobin concentration considering the recent suggestion of the negative effect of ESAs.
10 Four trials have evaluated multiple patient-reported outcomes and quality of life indices. Although some individual measures showed improvement, the overall quality of life effects have been small and inconsistent. The Normal Hematocrit Study showed a significant improvement on the physical-functioning scale of the Medical Outcomes Study 36-Item Short-Form General Health Survey (SF-36) but no significant effects on any of its other seven scales. The CHOIR Trial [7] did not show a significant improvement in any scale of the SF-36 Instrument in the High- Haemoglobin Group compared with the Low- Haemoglobin Group. The CREATE study [8] seems to be an outlier because quality of life deteriorated in the lower Hb arm and improved in patients assigned to the higher Hb. The TREAT study [9] showed a significant effect on the Functional Assessment of Cancer Therapy Fatigue Instrument but not on quality of life assessments based on the SF-36.