Transcription of BuTrans Patch - RxFiles
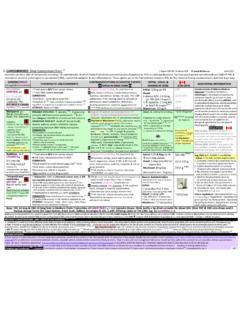
1 RxFiles Q&A Summary: Buprenorphine Transdermal Patch Pg 1 BuTrans Patch Buprenorphine Transdermal System (BTDS) for Weekly Application Classification1,2 {Semisynthetic, highly lipophilic opioid; derivative of morphine alkaloid thebaine; brain tissue levels far exceed serum levels} o Opioid analgesic (mu agonist; kappa & delta antagonist). Narcotic and Controlled Drug (Canada). It is often considered a partial mu agonist; however some recent literature suggests full potent mu Its action may more resemble a full mu agonist at lower doses, and partial mu agonist at higher doses. Controversial! {Note, a related product, SUBOXONE consists of [buprenorphine 2mg + naloxone an opioid antagonist ] as a SL tablet used to treat opioid dependence. Bioavailability of buprenorphine-variable: Transdermal 15%; SL= 30%-70%; Suboxone dosage range is 4-24mg/day buprenorphine.}
2 The amount of buprenorphine in 4 mg SL may equate to the amount in 16 BuTrans -20 patches. Only about 3% of the naloxone in Suboxone is absorbed; it will precipitate withdrawal if injected; useful in addiction med.} Strengths o Patch (matrix): 5mcg/hr ( ), 10mcg/hr ( ), 20mcg/hr ( ) Use/Place in Therapy o Persistent pain of moderate intensity in adults ( 40kg) requiring continuous opioid analgesia for an extended period of time (not suitable for unstable or widely fluctuating pain). [Higher Patch strengths TRANSTEC 35-70mcg/hr (q3d) available in Europe for ] o Can be used in opioid na ve patients (alternate to codeine, tramadol) and patients previously only on prn opioids o Considered when non-opioids provide inadequate relief and strong opioids undesirable in chronic non-cancer pain Contraindications (CI), official 1 CPS o Hypersensitivity, GI (ileus, surgical abdomen), mild/intermittent/acute pain, acute asthma/obstructive airway/respiratory depression, acute alcoholism/dependence, opioid dependence/acute opioid withdrawal, convulsive disorders, MAOIs within 14 days, myasthenia gravis, hepatic insufficiency, pregnancy/lactation; <40kg Dose { Patch provides sustained levels & analgesia over 7 days.
3 } {High affinity for mu receptor blockade may last >24hrs. Effect not totally related to plasma levels.} o Begin at: 5mcg/hr Patch applied once weekly; titrate up as necessary or if previously on opioid (up to 80mg oral morphine equivalent/day) may start on 5-10mcg/hr Patch once weekly (medication for breakthrough pain should also be provided) o Dose adjustments: generally recommended after 7 days; and not more frequently than after 3 days. o Maximum dose: 20mcg/hr. ( Patch applied for 7 days.) Doses 40mcg/hr may be associated with QT prolongation (but less than methadone)!5 o Breakthrough pain: may be managed by acetaminophen or NSAID +/- codeine or other breakthrough meds prn o Adjustments: Renal dysfx: NO dose adjustment required; (hepatic metabolism glucuronidation & biliary excretion).
4 Administration o Apply to: non-irritated, dry, intact skin; upper outer arm, upper chest, upper back or side of chest (always above the umbilicus) o Do not apply creams or ointments etc. to skin < 6hours prior to Patch application as may affect adhesion. o If site irritation, consider a corticosteroid spray ( beclomethasone or fluticasone) to skin area prior to Patch ; (this lacks data & may affect absorption). {Alternately, steroid cream post- Patch or well in advance (> 6-12hr) of Patch application.} o Rotate sites with each new Patch ; choose 4 or more sites and rotate; allow 3 weeks before reusing the same site o Avoid exposure of Patch to direct sunlight ( absorption). Showering, swimming & bathing should not affect Patch . Drug Interactions (DI) Metabolized via CYP3A4 to nor-buprenorphine (an active metabolite).
5 O 3A4 inhibitors: dose related toxicity of buprenorphine amiodarone, itraconazole, clarithromycin, fluconazole, erythromycin, grapefruit juice, protease inhibitors ritonavir, nelfinavir, amprenavir, verapamil, diltiazem o 3A4 inducers: likely to efficacy of buprenorphine: phenobarbital, carbamazepine, phenytoin, rifampin o CNS depressants: additive effects ( sedation, alertness, confusion, dizziness) o alcohol, benzodiazepines, sedative/hypnotics, antipsychotics, antihistamines o Other: Warfarin INR; anesthetics hepatic blood flow & [buprenorphine]; Benzodiazepines flunitrazepam: deaths reported in addict population Adverse Events (AE) {Most are similar to other opioids.} o Common on initiation: nausea45%, dizziness27%, somnolence24%, constipation21%, pruritus, dry mouth o Most common in clinical trials (rates from crossover trials; for difference from placebo rates, see CPS or specific trial literature): o anorexia, application site erythema/pruritis25%, asthenia, constipation, dizziness27%, dry mouth, headache, hyperhydrosis16%, insomnia, nausea +/- vomiting, somnolence.
6 [Potential QT prolongation with 40mcg/hr Patch .] o Serious, but less common with careful dose titration: respiratory depression however ceiling effect in resp depression, hypotension Discontinuing / Withdrawal o Consider tapering if higher doses to reduce withdrawal symptoms; withdrawal generally mild & resolves in 2 weeks o After removal of Patch , levels decline gradually; ~ 50% over ~12hours (10-24 hrs); administering a subsequent opioid after Patch removal should generally be delayed until 24hours after removal Other Cost / 4 weeks: 5mcg/hr: $ 60 10mcg/hr: $ 105 20mcg/hr: $ 185 (includes markup & dispensing fee) Currently not covered by most drug plans! o Steady state levels in ~3 days. Heat sources (external): will absorption & risks ( heat pad, hot bath, sauna, sunbathing, fever, etc.)
7 O Advantages: long action useful for chronic-stable type pain; once weekly application & kappa antagonist effect may result in less dsyphoria, psychological craving & dependence {However, data from Norway suggests addiction concerns}6. May cause less withdrawal when stopped than other opioids; incidence of constipation may be lower. Compared to the fentanyl Patch : lower abuse potential, mild withdrawal symptoms, may initiate in opioid na ve. o Disadvantages: long & delayed action means it is not suitable for acute or fluctuating pain; adverse effects may be sustained for 24 hours after removal of Patch .{If one holds that it is a partial mu agonist, this would limit the opioid effect resulting in both a ceiling dose & potential withdrawal in patients dependent on other long-term opioids.}
8 }. Studies are short term ( 12 weeks; most 4weeks); results modest & benefits harms (NNT = 7-8 & NNH for AE = 6-9). o CEDAC (Sept-2011 CDR Update): recommends against listing for coverage; high cost but no more effective than PO opioids Estimated Dose Equivalencies: BuTrans (BTDS) may be 25 110x more potent than oral morphine; individual variance; highly controversial!!!7 Daily Opioid Dose* 1,5,8,9 & Approximate Cost/4wks Acetaminophen + Codeine (30mg) Caffeine 6 (x30mg) tabs 7-8 (x30mg) tabs $43 Codeine 100mg 200 mg $67 400 mg $89 Tramadol - 150 mg $56 300 mg $100 Oral Morphine 15 mg 30 mg $30 60 mg $42 Oral Oxycodone 10 mg 15 20 mg $64 30 -40 mg $92 Oral Hydromorphone mg 6 mg $51 12 15 mg $72 Fentanyl Patch - - 12 mcg/hr $42 Initial BuTrans Patch dose if on previous opioid.
9 5 mcg/hr 5 mcg/hr + something for breakthru 5-10 mcg/hr + something for breakthru Estimate of Eventual BuTrans Patch Strength 5 mcg/hr $60 10 mcg/hr $10520 mcg/hr * $185 Note however that opioid withdrawal may occur for patients taking long-term and/orhigher doses of opioidsafter switching to buprenorphine!** *Monograph does not recommend starting > than 10 mcg/hr (as per dosing above). Table serves as a guide; actual dosing requires careful individualization & reassessment! ** Can patients on high doses of morphine &/or strong opioids be switched to transdermal buprenorphine? (See also extras under page 3 of this Q&A online.) Currently this is not recommended in Canada and there is concern about opioid withdrawal. However, one study successfully switched cancer patients on oral morphine (120-240mg/d) and transdermal fentanyl (50-100mcg/hr) to BTDS using a potency ratios of 70:1 for morphine and for transdermal fentanyl.
10 10 Note, due to transdermal route, there is less bioavailability variance than oral opioids. Anecdotally, some physicians report success with direct switching of <40-60mg/day morphine equivalent opioid regimens. Approach 1: wean patient over several weeks to about half their opioid dose, then convert to estimated equivalent buprenorphine dose +/- fast acting opioid. Approach 2: Apply first dose of equivalent dose buprenorphine Patch at same time as taking last dose of long-acting opioid +/- fast acting opioid. Cost/week based on lowest cost sustained release (SR) formulations. RxFiles Q&A Summary: Buprenorphine Transdermal Patch Pg 2 \ Table 1: Randomized controlled trials (RCT): buprenorphine transdermal system (BTDS) - BuTrans (7 day) Patch , chronic non-cancer pain Patients Intervention Results (primary; other) Comments (General: industry sponsored trials) Low back pain, mod-sev (VAS 2/5) for 6wks & not well controlled.