Transcription of Effects of Nonsteroidal Antiinflammatory Drugs on Platelet ...
1 THERAPEUTIC REVIEW. Effects of Nonsteroidal Antiinflammatory Drugs on Platelet Function and Systemic Hemostasis Andrew I. Schafer, MD. Aspirin and nonaspirin Nonsteroidal Antiinflammatory Drugs (NSAIDsJ inhibit Platelet cyclooxygenase, thereby blocking the formation of thromboxane A2 These Drugs produce a systemic bleeding tendency by impairing thromboxane-dependent Platelet aggregation and consequently prolonging the bleeding time. Aspirin exerts these Effects by irrevers . ibly blocking cyclooxygenase and, therefore, its actions persist for the circulating lifetime of the Platelet . Nonaspirin NSAIDs inhibit cyclooxygenase reversibly and, therefore, the duration of their action depends on specijic drug dose, serum level, and half-life. The clinical risks of bleeding with aspirin or non aspirin NSAIDs are enhanced by the concom- itant use of alcohol or anticoagulants and by associated conditions, including advanced age, liver disease, and other coexisting coagulopathies.)
2 N provide onsteroidal Antiinflammatory Drugs (NSAIDs). effective relief of pain and inflammation normality in platelets. This paper reviews Effects of NSAIDs on Platelet function and compares and con- caused by a variety of clinical disorders, including trasts actions of aspirin and nonaspirin NSAIDs. In different types of arthritis, nonarthritic musculoskel- addition, guidelines for identifying patients at risk of etal conditions, headache, and dysmenorrhea. More bleeding from aspirin and nonaspirin NSAIDs and than 70 million prescriptions for NSAIDs (excluding suggestions for alternative analgesics are provided. aspirin) were written in the United States in 1991, predominantly for these disorders, thus generating Platelet -VESSEL WALL INTERACTIONS. a per capita consumption of prescriptions per 1,000 people and a retail cost exceeding $ billion. 1 A monolayer of endothelial cells lines the intimal Because of increased physician awareness of ad- surface of blood vessels throughout the circulatory verse gastrointestinal events among NSAID users, 2 a tree, and under normal circumstances, these cells stabilization of NSAID usage and an increased use of maintain blood fluidity by providing a thromboresis- gastroprotective and anti-ulcer Drugs have occurred.
3 Tant surface. Anticoagulant factors of endothelial Whereas most physicians find NSAIDs to be safe and cells include prostacyclin (PGI 2), an eicosanoid prod- effective, gastroenterologists have been increasingly uct of arachidonic acid metabolism, and nitric oxide, concerned about their toxic Effects on the gut, the a component of endothelium-derived relaxing factor most significant of which is gastrointestinal hemor- (EDRF). 6 7 Prostacyclin and nitric oxide maintain rhage. a-s The risk of gastrointestinal bleeding from blood cells in a quiescent state by inducing vasore- NSAIDs is compounded by their adverse Effects on laxation and inhibiting platelets. Prostacyclin stimu- systemic coagulation resulting in a qualitative ab- lates adenylyl cyclase and raises the level of cyclic AMP in vascular smooth muscle cells and platelets. Nitric oxide stimulates guanylyl cyclase and raises levels of cyclic GMP in the same cell types. From the Department of Medicine, Baylor College of Medicine, Hous- At a site of vascular injury, thromboresistant prop- ton, and the Medical Service, Houston Veterans Affairs Medical Center.
4 Erties of endothelial cells are lost or impaired, and Houston Texas. Address for reprints: Andrew I. Schafer, MD, Medical thrombogenic subendothelial components of the Service (111), Houston VA Medical Center, 2002 Holcombe Blvd., vessel wall ( , collagen) become exposed to blood. Houston, TX 77030. Platelets attach to the damaged vessel wall through a J Clln Pharmacol1995;35:209-219 209. Downloaded from by guest on May 25, 2011. SCHAFER. lipid pools by phospholipases (phospholipase A2 or the sequential actions of phospholipase C and diglyc- eride lipase), which are activated by various extra- cellular stimuli. Cyclooxygenases then catalyze the oxygenation of free arachidonic acid to cyclic endo- peroxide prostaglandin G2 (PGG2 ), which is subse- quently converted by hydroperoxidase to PGH2. (In platelets, arachidonic acid is also oxygenated by a 12- lipoxygenase to form 12-hydroperoxy- and 12-hy- droxy-fatty acids, which have uncertain biologic roles.)
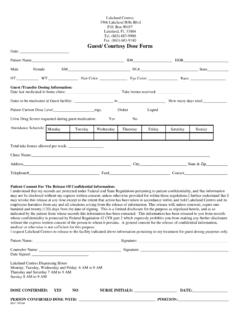
5 Subsequently, cells selectively differentiate in their metabolism of cyclic endoperoxides to biologi- cally active products ( , via thromboxane synthase to thromboxane A2 in platelets, or via prostacyclin synthase to prostacyclin in endothelial cells). Platelet -derived thromboxane A2 and endothe- lium-derived prostacyclin and nitric oxide have di- rectly opposing actions on platelets and the vessel wall. Platelet -derived thromboxane A2 is a potent Figure 1. Platelet and vessel wall eicosanoid metabolism. Platelets Platelet activator and vasoconstrictor, and endothe- and vascular endothelial cells are stimulated by a variety of posi- lium-derived prostacyclin and nitric acid are Platelet tive stimuli (agonists) to activate phospholipases, which hydrolyze inhibitors and vasodilators. The balance of their pro- free arachidonic acid from their membrane phospholipid pools. duction represents an important determinant of the Free arachidonic acid is then oxygenated to prostaglandin endo- state of Platelet -vessel wall interactions, blood fluid- peroxides in both cell types by cyclooxygenase, an enzyme that is irreversibly inhibited by aspirin and reversibly inhibited by non- ity, and hemostasis.
6 Both in vitro 10-13 and in vivo 14- 16. aspirin NSAlDs. (In platelets, arachidonic acid is also metabolized studies demonstrate that activated platelets unidi- to 12-HPETE and 12-HETE by a 12-lipoxygenase, but the physiolog- rectionally divert endoperoxides to vascular cells ical significance of this pathway is unclear.) The labile endoperox- (termed "endoperoxide steal") to serve as substrates ides, PGG 2 and PGH2 , are then metabolized by thromboxane syn- thase to thromboxane A2 in platelets. and by prostacyclin synthase for prostacyclin synthase (Figure 1). This endoperox- to prostacyclin (PGI2) in endothelial cells. Activated platelets can ide rediversion increases prostacyclin production at also divert their endoperoxides to endothelial cells and augment the Platelet -vascular interface presumably as a prostacyclin formation. Prostacyclin is a potent Platelet inhibitor thromboresistant response to activated platelets. (and vasodilator) that exerts this action by raising Platelet intracel- lular cyclic AMP levels.
7 Thromboxane A2 is a potent Platelet acti- vator (and vasoconstrictor) that exerts this action by decreasing (or INHIBITION OF CYCLOOXYGENASE BY. preventing the elevation ofJ intracellular cyclic AMP levels. ASPIRIN AND NONASPIRIN NSAIDs Aspirin covalently acetylates the active site Ser529. process of Platelet "adhesion" mediated by the bind- of cyclooxygenase and irreversibly inhibits the en- ing of von Willebrand factor to its Platelet receptors It might be expected that simultaneous on membrane glycoprotein (Gp) lb. Binding of von inactivation of Platelet and endothelial cyclooxygen- Wille brand factor to Platelet Gp lb initiates a cascade ase by aspirin would have deleterious Effects on he- of intracellular signals8 that stimulates the "release mostasis by blocking thromboxane A2 and prostacy- reaction." Major products of this Platelet release re- clin formation. However, to enhance selectivity of action are prepackaged contents ( , ADP) of spe- aspirin inhibition on Platelet thromboxane A2 syn- cific granules and thromboxane A2 , which is synthe- thesis, several therapeutic strategies have been pro- sized de novo from arachidonic acid in response to posed to exploit pharmacokinetic differences be- Platelet activation.)
8 Products of the Platelet release tween Effects of aspirin on Platelet and endothelial reaction then act in concert to promote Platelet ag- cyclooxygenase. First, cyclooxygenase acetylation gregation, which results in formation of an occlusive by aspirin permanently inactivates the enzyme in Platelet plug at the vascular injury site. anucleate platelets, which normally have a circulat- The principal cyclooxygenase metabolites of ara- ing lifetime of 7 to 10 days. Recovery of Platelet chidonic acid are thromboxane A2 in platelets and thromboxane A2 synthesis in an individual exposed PGI2 in endothelial cells9 (Figure 1). The rate-limiting to aspirin requires that senescent, cyclooxygenase- step in production of these metabolites is hydrolysis inhibited platelets be replaced in the circulation of free arachidonic acid from membrane phospho- with new, uninhibited platelets from bone marrow 210 J Clln Pharmacol1995;35:209-219. Downloaded from by guest on May 25, 2011.
9 Effects OF NSAIDS ON Platelet FUNCTION AND SYSTEMIC HEMOSTASIS. megakaryocytes not exposed to the drug. In contrast, vascular endothelial cells recover rapidly after aspi- rin exposure because they can continuously synthe- size new, unacetylated cyclooxygenase. 24 This difference in protein synthetic capacities of the two cell types has led to suggestions that alternate-day administration may optimize the antithrombotic po- tential of aspirin by maintaining essentially continu- ous suppression of Platelet thromboxane A2 produc- tion while permitting intermittent recovery of endo- thelial prostacyclin production. A second difference between cyclooxygenases of the two cell types is in- creased sensitivity of Platelet cyclooxygenase to as- Figure 2. Patterns of Platelet aggregation in vitro induced by ADP, pirin. 25 26 Consistent with in vitro observations is the epinephrine, collagen, and arachidonate. The upper series of trac- finding that administration of very low doses of aspi- ings depicts normal aggregation patterns; the lower series shows rin to healthy subjects results in cumulative inhibi- changes in aggregation in response to the corresponding stimuli in individuals taking aspirin and nonaspirin NSAIDs.
10 Tion of Platelet thromboxane production. 27 28 How- ever, long-term administration of conventionally for- mulated aspirin at low doses partially suppresses vascular prostacyclin formation. 29 30 Therefore, bio- Platelet -rich plasma prepared from freshly drawn chemical selectivity of this regimen for platelets is at blood. Aggregation in the stirred samples of Platelet - best relative, not absolute. 31 32 Finally, strategies with rich plasma is then measured by monitoring the in- low-dose, controlled-release, and enteric-coated crease in light transmission that occurs as platelets preparations of aspirin provide a drug delivery rate clump. Tracings of normal aggregation responses to that does not exceed the threshold for hepatic ex- various Platelet agonists are shown in the top row of traction of aspirin, thus leading to first-pass metabo- Figure 2. An initial depression in the baseline that is lism of aspirin to salicylate, a very weak and revers- caused by a transient decrease in light transmission ible inhibitor of cyclooxygenase.