Transcription of ESPEN guideline on clinical nutrition and hydration in ...
1 ESPEN GuidelineESPEN guideline on clinical nutrition and hydration in geriatricsDorothee Volkerta,*, Anne Marie Beckb, Tommy Cederholmc, Alfonso Cruz-Jentoftd,Sabine Goissere, Lee Hooperf, Eva Kiesswettera, Marcello Maggiog,h,Agathe Raynaud-Simoni, Cornel C. Siebera,j, Lubos Sobotkak, Dieneke van Asseltl,Rainer Wirthm, Stephan C. BischoffnaInstitute for Biomedicine of Aging, Friedrich-Alexander-Universit at Erlangen-N rnberg, Nuremberg, GermanybDietetic and Nutritional Research Unit, Herlev and Gentofte University Hospital, University College Copenhagen, Faculty of Health, Institute of Nutritionand Nursing, Copenhagen, DenmarkcDepartment of Public Health and Caring Sciences, Division of clinical nutrition and Metabolism, Uppsala University, Uppsala, SwedendServicio de Geriatr a, Hospital Universitario Ram on y Cajal (IRYCIS)
2 , Madrid, SpaineNetwork Aging Research (NAR), University of Heidelberg, Heidelberg, GermanyfNorwich Medical School, University of East Anglia, Norwich, UKgDepartment of Medicine and Surgery, University of Parma, Parma, ItalyhGeriatric-Rehabilitation Department, Parma University Hospital, Parma, ItalyiDepartment of Geriatrics, Bichat University Hospital APHP, Faculty of Medicine Denis Diderot, Paris, FrancejKrankenhaus Barmherzige Br der, Regensburg, GermanykDepartment of Medicine, Medical Faculty and Faculty Hospital Hradec Kralove, Charles University, Prague.
3 Czech RepubliclDepartment of Geriatric Medicine of the Radboud University Medical Center, Nijmegen, The NetherlandsmMarien Hospital Herne, Ruhr-Universit at Bochum, Herne, GermanynInstitute of Nutritional Medicine, University of Hohenheim, Stuttgart, Germanyarticle infoArticle history:Received 21 May 2018 Accepted 29 May 2018 Keywords:GuidelineRecommendationsGeriatr icsNutritional careMalnutritionDehydrationsummaryBackgr ound:Malnutrition and dehydration are widespread in older people, and obesity is an increasingproblem.
4 In clinical practice, it is often unclear which strategies are suitable and effective in counter-acting these key health :To provide evidence-based recommendations for clinical nutrition and hydration in older personsin order to prevent and/or treat malnutrition and dehydration. Further, to address whether weight-reducing interventions are appropriate for overweight or obese older :This guideline was developed according to the standard operating procedure for ESPEN guidelines and consensus papers. A systematic literature search for systematic reviews and primarystudies was performed based on 33 clinical questions in PICO format.
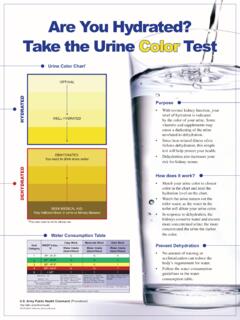
5 Existing evidence was gradedaccording to the SIGN grading system. Recommendations were developed and agreed in a multistageconsensus :We provide eighty-two evidence-based recommendations for nutritional care in older persons,covering four main topics: Basic questions and general principles, recommendations for older personswith malnutrition or at risk of malnutrition, recommendations for older patients with specific diseases,and recommendations to prevent, identify and treat dehydration. Overall, we recommend that all olderpersons shall routinely be screened for malnutrition in order to identify an existing risk early.
6 Oralnutrition can be supported by nursing interventions, education, nutritional counseling, food modificationand oral nutritional supplements. Enteral nutrition should be initiated if oral, and parenteral if enteralnutrition is insufficient or impossible and the general prognosis is altogether favorable. Dietary re-strictions should generally be avoided, and weight-reducing diets shall only be considered in obese olderpersons with weight-related health problems and combined with physical exercise. All older personsshould be considered to be at risk of low-intake dehydration and encouraged to consume adequateAbbreviations:ADL, activities of daily living; BM, biomedical endpoint; EN, enteral nutrition ; GPP, good practice point; MoW, meals on wheels; ONS, oral nutritionalsupplements; PC, patient-centered endpoint; PICO, population of interest, interventions, comparisons, outcomes; PN, parenteral nutrition ; RCT, randomized controlled trial;SLR, systematic literature review.
7 *Corresponding Volkert).Contents lists available atScienceDirectClinical Nutritionjournal homepage: 2018 European Society for clinical nutrition and Metabolism. Published by Elsevier Ltd. All rights nutrition 38 (2019) 10e47amounts of drinks. Generally, interventions shall be individualized, comprehensive and part of amultimodal and multidisciplinary team :A range of effective interventions is available to support adequate nutrition and hydration inolder persons in order to maintain or improve nutritional status and improve clinical course and qualityof life.
8 These interventions should be implemented in clinical practice and routinely used. 2018 European Society for clinical nutrition and Metabolism. Published by Elsevier Ltd. All Particularities of older personsAn older person is usually defined as a person aged 65 years orolder. A geriatric patient is not specifically age-defined but rathercharacterized by a high degree of frailty and multiple active dis-eases which becomes more common in the age group above 80years[1]. As a consequence of acute and/or chronic disease incombination with age-related degenerative changes, limitations inphysical, mental and/or social functions occur.
9 The ability toperform the basic activities of daily living independently is jeop-ardized or lost. The person is in increased need of rehabilitative,physical, psychological and social care and requires a holisticapproach to avoid partial or complete loss of independence[1].It is the main aim of geriatric medicine to optimize functionalstatus of the older person and, thus, to ensure greatest possibleautonomy and best possible quality of life[1]. A reduced adaptiveand regenerative capacity, however, and thus, reduced capacity forrehabilitation is characteristic of older patients, making it moredifficult to return the patient to an unrestricted or to his/her pre-vious of the most meaningful geriatric syndromes is sarcopenia,characterized by a disproportionate loss of muscle mass andstrength that is accompanied by a decline in physical activity,functionality and performance.
10 An excessive loss of muscle massand strength results in physical impairment, frailty, disability anddependence from others. Sarcopenia also impairs the metabolicadaptation to stress and disease[2]. Despite large overlap withsarcopenia, frailty represents a distinct clinical syndrome, charac-terized by an increased vulnerability to stress as a consequence ofcumulative decline in many physiological systems during is associated with an increased risk of adverse health out-comes and estimated to affect about 25% of persons aged 85 yearsor older[3,4].