Transcription of Food and mood: how do diet and nutrition affect mental ...
1 Food for Thought 2020. Food and mood: how do diet and nutrition affect BMJ: first published as on 29 June 2020. Downloaded from on 11 January 2022 by guest. Protected by copyright. mental wellbeing? Poor nutrition may be a causal factor in the experience of low mood, and improving diet may help to protect not only the physical health but also the mental health of the population, say Joseph Firth and colleagues D. epression and anxiety are the experiences. In addition, relationships load, and the resultant compensatory most common mental health between nutrition and longstanding mental responses, could lower plasma glucose to conditions worldwide, mak illness are compounded by barriers to concentrations that trigger the secretion of ing them a leading cause of maintaining a healthy diet . These barriers autonomic counter-regulatory hormones Even beyond diag disproportionality affect people with such as cortisol, adrenaline, growth nosed conditions, subclinical symptoms of mental illness and include the financial hormone, and 9 The potential depression and anxiety affect the wellbeing and environmental determinants of health, effects of this response on mood have been and functioning of a large proportion of the and even the appetite inducing effects of examined in experimental human research Therefore, new approaches to psychiatric of stepped reductions in plasma glucose managing both clinically diagnosed and While acknowledging the complex, concentrations conducted under laboratory subclinical depression and anxiety are multidirectional nature of the relationships conditions through glucose perfusion.
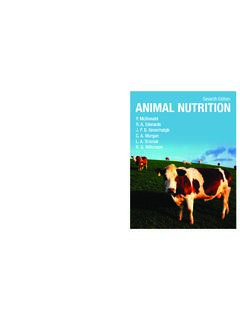
2 Needed. between diet and mental health (fig 1), in These findings showed that such counter- In recent years, the relationships bet this article we focus on the ways in which regulatory hormones may cause changes ween nutrition and mental health have certain foods and dietary patterns could in anxiety, irritability, and In gained considerable interest. Indeed, affect mental health. addition, observational research has found epidemiological research has observed that recurrent hypoglycaemia (low blood that adherence to healthy or Mediterranean Mood and carbohydrates sugar) is associated with mood dietary patterns high consumption of Consumption of highly refined carbohy The hypothesis that repeated and fruits, vegetables, nuts, and legumes; drates can increase the risk of obesity and rapid increases and decreases in blood moderate consumption of poultry , eggs, Glycaemic index is a relative glucose explain how consumption and dairy products; and only occasional ranking of carbohydrate in foods accord of refined carbohydrate could affect consumption of red meat is associated ing to the speed at which they are digested, psychological state appears to be a good with a reduced risk of However, absorbed, metabolised, and ultimately fit given the relatively fast effect of diets the nature of these relations is complicated affect blood glucose and insulin levels.
3 As with a high glycaemic index or load on by the clear potential for reverse causality well as the physical health risks, diets with depressive symptoms observed in human between diet and mental health (fig 1). For a high glycaemic index and load (eg, diets However, other processes may example, alterations in food choices or containing high amounts of refined carbo explain the observed relationships. For preferences in response to our temporary hydrates and sugars) may also have a det instance, diets with a high glycaemic psychological state such as comfort rimental effect on psychological wellbeing; index are a risk factor for diabetes, 5. foods in times of low mood, or changes in data from longitudinal research show an which is often a comorbid condition with appetite from stress are common human association between progressively higher depression. 4 11 While the main models dietary glycaemic index and the incidence of disease pathophysiology in diabetes of depressive Clinical studies and mental illness are separate, common Key Messages have also shown potential causal effects abnormalities in insulin resistance, brain of refined carbohydrates on mood; experi volume, and neurocognitive performance Healthy eating patterns, such as mental exposure to diets with a high gly in both conditions support the hypothesis the Mediterranean diet , are associ- caemic load in controlled settings increases that these conditions have overlapping ated with better mental health than depressive symptoms in healthy volunteers, pathophysiology.
4 12 Furthermore, the unhealthy eating patterns, such as with a moderately large inflammatory response to foods with a the Western diet Although mood itself can affect our high glycaemic index13 raises the possibility The effects of certain foods or die- food choices, plausible mechanisms exist that diets with a high glycaemic index are tary patterns on glycaemia, immune by which high consumption of processed associated with symptoms of depression activation, and the gut microbiome carbohydrates could increase the risk of through the broader connections between may play a role in the relationships depression and anxiety for example, mental health and immune activation. between food and mood through repeated and rapid increases More research is needed to under- and decreases in blood glucose. Measures diet , immune activation, and depression stand the mechanisms that link food of glycaemic index and glycaemic load Studies have found that sustained adher . and mental wellbeing and determine can be used to estimate glycaemia and ence to Mediterranean dietary patterns how and when nutrition can be used insulin demand in healthy individuals can reduce markers of inflammation in to improve mental health after Thus, high dietary glycaemic On the other hand, high calorie the bmj | BMJ 2020;369:m2440 | doi: 1.
5 Food for Thought 2020. Cravings, habits and Good quality diet Psychological in humans is associated with alterations situational factors and social factors of the gut microbiome,25 and transfer of BMJ: first published as on 29 June 2020. Downloaded from on 11 January 2022 by guest. Protected by copyright. For example: Healthy fats faecal gut microbiota from humans with Limited fast foods depression into rodents appears to induce Multiple Fruits and vegetables Hormonal, animal behaviours that are hypothesised biological High bre foods in ammatory, pathways neural pathways to indicate depression-like 26 Such findings suggest a role of altered neuroac . Physical health mental health tive microbial metabolites in depressive symptoms. For example: For example: Insulin sensitivity Better mood In addition to genetic factors and Less cardiovascular risk Determinants of physical and mental comorbidity Less stress exposure to antibiotics, diet is a potentially Healthy weight Lower risk of illness modifiable determinant of the diversity, Other health behaviours Cognitive function relative abundance, and functionality of the gut microbiome throughout life.
6 For Fig 1 | Hypothesised relationship between diet , physical health, and mental health. The dashed instance, the neurocognitive effects of the line is the focus of this article. Western diet , and the possible mediating role of low grade systemic immune meals rich in saturated fat appear to stim people treated, and that giving omega-3 activation (as discussed above) may result ulate immune 15 Indeed, the fatty acids, which have anti-inflammatory from a compromised mucus layer with or inflammatory effects of a diet high in calo properties, before the medication seems without increased epithelial permeability. ries and saturated fat have been proposed to prevent the onset of cytokine induced Such a decrease in the function of the gut as one mechanism through which the West barrier is sometimes referred to as a leaky ern diet may have detrimental effects on However, the complexity of the hypo gut and has been linked to an unhealthy . brain health, including cognitive decline, thesised three way relation between gut microbiome resulting from a diet low hippocampal dysfunction, and damage diet , inflammation, and depression in fibre and high in saturated fats, refined to the blood-brain Since various is compounded by several important sugars, and artificial 23 27.
7 mental health conditions, including mood modifiers. For example, recent clinical Conversely, the consumption of a diet high disorders, have been linked to heightened research has observed that stressors in fibres, polyphenols, and unsaturated inflammation,16 this mechanism also pre experienced the previous day, or a personal fatty acids (as found in a Mediterranean sents a pathway through which poor diet history of major depressive disorders, diet ) can promote gut microbial taxa which could increase the risk of depression. This may cancel out the beneficial effects of can metabolise these food sources into hypothesis is supported by observational healthy food choices on inflammation anti-inflammatory metabolites,15 28 such studies which have shown that people and Furthermore, as heightened as short chain fatty acids, while lowering with depression score significantly higher inflammation occurs in only some the production of secondary bile acids on measures of dietary inflammation, 3 17 clinically depressed individuals, anti- and p-cresol.
8 Moreover, a recent study characterised by a greater consumption inflammatory interventions may only found that the ingestion of probiotics by of foods that are associated with inflam benefit certain people characterised by healthy individuals, which theoretically mation (eg, trans fats and refined carbo an inflammatory phenotype, or those target the gut microbiome, can alter the hydrates) and lower intakes of nutritional with comorbid inflammatory brain's response to a task that requires foods, which are thought to have anti- Further interventional research is needed emotional attention29 and may even reduce inflammatory properties (eg, omega-3 fats). to establish if improvements in immune symptoms of When viewed However, the causal roles of dietary inflam regulation, induced by diet , can reduce together, these studies provide promising mation in mental health have not yet been depressive symptoms in those affected by evidence supporting a role of the gut established. inflammatory conditions.
9 Microbiome in modulating processes that Nonetheless, randomised controlled regulate emotion in the human brain. trials of anti-inflammatory agents (eg, Brain, gut microbiome, and mood However, no causal relationship between cytokine inhibitors and non-steroidal A more recent explanation for the way in specific microbes, or their metabolites, anti-inflammatory drugs) have found which our food may affect our mental well and complex human emotions has been that these agents can significantly being is the effect of dietary patterns on the established so far. Furthermore, whether reduce depressive Specific gut microbiome a broad term that refers to changes to the gut microbiome induced nutritional components (eg, polyphenols the trillions of microbial organisms, includ by diet can affect depressive symptoms or and polyunsaturated fats) and general ing bacteria, viruses, and archaea, living clinical depressive disorders, and the time dietary patterns (eg, consumption of a in the human gut.)
10 The gut microbiome in which this could feasibly occur, remains Mediterranean diet ) may also have anti- interacts with the brain in bidirectional to be shown. inflammatory effects,14 19 20 which raises the ways using neural, inflammatory, and possibility that certain foods could relieve hormonal signalling The role Priorities and next steps or prevent depressive symptoms associated of altered interactions between the brain In moving forward within this active field with heightened inflammatory A and gut microbiome on mental health has of research, it is firstly important not to recent study provides preliminary support been proposed on the basis of the follow lose sight of the wood for the trees that for this The study shows that ing evidence: emotion-like behaviour in is, become too focused on the details and medications that stimulate inflammation rodents changes with changes in the gut not pay attention to the bigger questions. typically induce depressive states in microbiome,24 major depressive disorder Whereas discovering the anti-inflammatory 2 doi: | BMJ 2020;369:m2440 | the bmj Food for Thought 2020.