Transcription of Joint British Diabetes Societies for Inpatient Care Group
1 Self-management ofdiabetes in hospitalJoint British Diabetes Societies for Inpatient care GroupMarch 2012 Supporting, Improving, Caring3 Foreword41. Main recommendations62. Introduction73. The role of the Diabetes specialist team94. Self-management of Diabetes with insulin10 Criteria for self-management10 Staff responsibilities11 Planning elective admissions12 Patient education12 Dispensing and storage of insulin12 Checking and recording patient self-administration of medicines13 Blood glucose monitoring in hospital13 Management of hypoglycaemia and hyperglycaemia14 Content and timing of meals145. Self-management of insulin pumps (continuous subcutaneous 15insulin infusion [CSII] during hospital admission)6. Self-administration of other Diabetes medication167. Audit standards178. References189. Appendices20 Appendix 1: Agreement to self-manage Diabetes during hospital admission20 Appendix 2: Patient information leaflet21 Appendix 3: Information for healthcare professionals22 Insulin self-management for adult inpatients with diabetes22 Appendix 4: Self-administration levels adapted from the Nursing and Midwifery Council (2007)24 Appendix 5: Pump management for elective procedures under sedation 25or anaesthesiaAppendix 6: guidelines for insulin pump therapy in specific situations26 Contents4 ForewordThese guidelines have been commissioned by the Joint British Diabetes Societies for Inpatient care Groupin collaboration with NHS aim of the document is to improve the safety of the in hospital management of Diabetes .
2 Diabetescare is very individualised, especially if that person is using insulin. It follows that the person with thegreatest expertise in managing Diabetes is commonly the individual themselves. Allowing patients to selfmanage their Diabetes in hospital should significantly improve patient safety. The correct supportstructures need to be provided to ensure that this is properly monitored but this must be done withoutcreating unnecessary bureaucracy. Target audienceThese guidelines emphasise that, at all stages of care in hospital the patient should remain in charge oftheir Diabetes care unless there is a specific reason not to. It is hoped that they will be of use to allhealthcare professionals who are involved in the delivery of Diabetes care in hospital. The target audiencespecifically includes: Ward nursing staff Ward pharmacists The Inpatient Diabetes specialist team Most importantly those involved in the writing and implementation of local Diabetes care policies.
3 Lead authorshipDr Daniel Flanagan, Plymouth Hospitals NHS Trust (Lead)Maggie Watkinson, Taunton and Somerset NHS Foundation Trust (Lead)Supporting organisationsEsther Walden (Norwich) Diabetes Inpatient Specialist Nurse (DISN) UK Group ChairProfessor Mike Sampson (Norwich) Joint British Diabetes Societies (JBDS) Inpatient care Group ChairDr Chris Walton, (Hull) Association of British Clinical Diabetologists (ABCD) ChairTracy Kelly, Diabetes UK 5 Writing groupDr Ketan Dhatariya, Norfolk and Norwich University Hospitals NHS Foundation TrustDr Anne Kilvert, Northampton General Hospital NHS TrustAlison Cox, Kings College Hospital NHS Foundation TrustCatherine Jenkins, The Whittington Hospital NHS TrustElly Baker, The Whittington Hospital NHS TrustJulie Worthington, Plymouth Hospitals NHS TrustLesley Lamen, Royal Liverpool and Broadgreen University Hospitals NHS TrustKathryn Leivesley, Liverpool Heart and Chest NHS Foundation TrustLinda Balian, Yeovil District Hospital NHS Foundation TrustMichelle Burke, South Eastern Health and Social care Trust, Northern IrelandPatricia Fairburn, York Teaching Hospital NHS Foundation TrustProfessor Sarah O Brien.
4 St Helens and Knowsley Teaching Hospitals NHS TrustHelen Davies (The Diabetes Management & Education Group of The British Dietetic Association)Natasha Jacques and Sally James (UK Clinical Pharmacy Association) Diabetes UK User Group - coordinated by Katie WilsonJBDS IP Review GroupDr Adrian Scott, Sheffield Teaching Hospitals NHS Foundation TrustDr Aled Roberts, Cardiff and Vale University NHS TrustDr Belinda Allan, Hull and East Yorks Hospital NHS TrustDr Chris Walton, Hull and East Yorks Hospital NHS TrustDebbie Stanisstreet, East and North Hertfordshire NHS TrustDr Gerry Rayman, The Ipswich Hospitals NHS TrustDr Johnny McKnight, NHS LothianDr Jonny Thow, York Teaching Hospital NHS Foundation TrustJune James, University Hospitals of Leicester NHS TrustDr Kate Richie, Southern Health and Social care Trust, Northern IrelandDr Louise Stuart, The Pennine Acute Hospitals NHS TrustDr Maggie Hammersley, Oxford University Hospitals NHS TrustDr Mark Savage, The Pennine Acute Hospitals NHS TrustDr Peter Winocour.
5 East and North Hertfordshire NHS TrustDr Rif Malik, King s College Hospital NHS Foundation TrustDr Rowan Hillson, MBE, National Clinical Director for DiabetesWith special thanks to Christine Jones (DISN UK Group administrator, Norwich) for her administrative workand help with these guidelines and with JBDS - IP61. Main recommendationsThe guiding principle of this document is that people with Diabetes managetheir condition on a day-to-day basis when out of hospital, and should continueto self-manage during a hospital admission unless there is a specific reason whythey cannot. The choice to continue to self-manage during admission, if wellenough to do so, should be that of the patient. This document details how thisdecision can be integrated with the rest of hospital care to provide safe andeffective management of Diabetes in hospital.
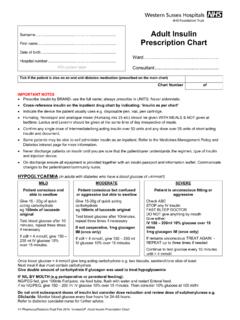
6 If ward staff are uncomfortablewith the patient s decision to self-manage, expert advice should be sought fromthe hospital Diabetes of diabetesis the process of deciding on and administering an insulin dose inresponse to self-measured capillary glucose values. Self-administrationis the taking of medication (injected or oral) as prescribed by a Trusts should provide written information toexplain the responsibilities of self-managementto both patients and hospital staff. 2. The responsible nurse and the patient shouldagree, on admission, the circumstances in whichthe patient should self-manage. An agreementform should be signed by both the patient and aregistered For elective surgical admissions, a care planshould be agreed at the pre-operativeassessment clinic to establish whether thepatient wishes to self-manage and thecircumstances in which this may not be possible.
7 4. During the admission, the clinical circumstancesshould be assessed regularly to ensure that thepatient s ability to self-manage has not beencompromised by their clinical The Diabetes specialist team should be involvedif there is disagreement about the patient sability to self-manage or if there are difficultieswith Diabetes control. Diabetes specialist nursestaffing levels should be sufficient to supportthis Patients should be able to self-monitor theirblood glucose but should make the resultsavailable to hospital staff. 7. The insulin dose administered by the patientshould be recorded on the prescription The hospital should ensure that the timing andcontent of meals are suitable for the patientwith Facilities should be available for the safe storageof insulin in the ward guideline has been produced by the JointBritish Diabetes Societies for Inpatient care Groupin collaboration with NHS Diabetes , and has beeninformed by user focus groups from Diabetes aims of the guideline are to improve inpatientexperience and safety for people with Diabetes .
8 Itis primarily aimed at healthcare professionalsworking in hospitals, although some aspects arerelevant to staff involved in pre-admissionpreparation. The guideline is designed to enableadaptation to local circumstances where required. BackgroundAll children, young people and adults admitted tohospital, for whatever reason, will receive effectivecare of their Diabetes . Wherever possible, they willcontinue to be involved in decisions concerning themanagement of their diabetesDiabetes National Service Framework1 Historically, people with Diabetes have often beenprevented from managing their own diabeteswhile in hospital. This has exposed them tomismanagement of their Diabetes as a result of: errors in the administration of insulin2 errors of Diabetes management inappropriate content and timing of meals mistreatment of hypoglycaemia misuse of variable-rate intravenous best, these errors lead to patient dissatisfaction,disempowerment and prolonged length of stay; atworst, patients may suffer serious harm or ,4In 2010 the National Diabetes InpatientAudit (NaDIA) reported that people with diabetesexperienced substantially longer hospital stays, poorglucose control, frequent medication errors andinsufficient contact with the Diabetes these factors contribute to the increasedcost of caring for inpatients with number of organisations have issued guidanceto address the problems associated with diabetescare in hospital.
9 The National Institute for Health and ClinicalExcellence (NICE) quality standard for inpatientcare6requires that People with diabetesadmitted to hospital are cared for byappropriately trained staff, provided with accessto a specialist Diabetes team, and given thechoice of self-monitoring and managing theirown insulin. The NHS Institute for Innovation andImprovement ThinkGlucose campaign developeda toolkit to improve quality of care of patients inhospital, including a decision tree for The National Patient Safety Agency (NPSA)issued guidance to reduce the number of errorsinvolving alert calling for staff training inuse of insulin. -Insulin passport to provide accurateinformation about insulin with Diabetes to be allowed toself-manage their Diabetes duringhospital admission wherever possible. NHS Diabetes introduced the e-learning modules Safe Use of Insulin 9and Safe Use ofIntravenous Insulin 10for staff training.
10 The Department of Health included insulinmaladministration in the never event task facing Diabetes specialist teams is tointegrate the policies listed above with localguidelines. Although this guideline focuses onself-management of insulin therapy, it alsoprovides guidance on other aspects of diabetesself-management. 2. Introduction8 Rationale for self-managementInsulin therapy remains a common cause ofuntoward incidents in hospitals. Problem areashighlighted by the NaDIA5include: prescription and administration of insulin timing of insulin administration in relation tomeals lack of knowledge among medical and nursingstaff managing patients with Diabetes lack of access to specialist advice about insulin-treated patients will have greaterknowledge and experience of insulin adjustmentthan the medical and nursing staff responsible fortheir will routinely monitor theircapillary glucose and adjust the insulin dosedepending on the result.