Transcription of NURSING CARE OF THE CLIENT HAVING TOTAL JOINT …
1 CHAPTER 39 / NURSING Care of clients with Musculoskeletal Disorders1243 NURSING CAREOF THE CLIENT HAVING TOTAL JOINT REPLACEMENTPREOPERATIVE CARE Assess the CLIENT s knowledge and understanding of theplanned operative procedure. Provide further explanationsand clarification as is important that the CLIENT have aclear and realistic understanding of the surgical procedure andexpected results. Knowledge decreases anxiety and increases theclient s ability to assist with postoperative care procedures. Obtain a NURSING history and physical assessment, includingrange of motion of the affected information not onlyallows nurses to tailor care to the needs of the individual but alsoserves as a baseline for comparison of postoperative assessmentdata.
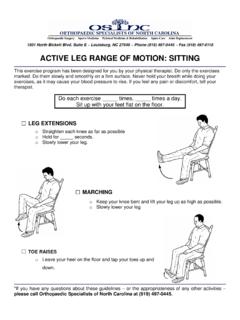
2 Explain necessary postoperative activity restrictions. Teachhow to use the overhead trapeze for changing who learns and practices moving techniques before surgerycan use them more effectively in the postoperative period. Provide or reinforce teaching of postoperative exercises spe-cific to the JOINT on which surgery is to be prescribed postoperatively to (a) strengthen muscles provid-ing JOINT stability and support, (b) prevent muscle atrophy andjoint contractures; and (c) prevent venous stasis and possiblethromboembolism. Teach respiratory hygiene procedures such as the use of incen-tive spirometry, coughing, and deep respi-ratory hygiene is imperative for all clients undergoing JOINT re-placement to prevent respiratory complications associated withimmobility and the effects of anesthesia.
3 In addition, many clientsundergoing TOTAL JOINT replacement are elderly and may have reduced mucociliary clearance. Discuss postoperative pain control measures, including use ofpatient-controlled analgesia (PCA) or epidural infusion as is important for the CLIENT to understand the purposeand use of postoperative pain control measures to allow earlymobility and reduce complications associated with immobility. Teach or provide prescribed preoperative skin preparationsuch as shower, shampoo, and skin scrub with antibacterial measures help reduce transient bacteria that maybe introduced into the surgical site. Administer intravenous antibiotic as therapyis initiated before or during surgery and continued postopera-tively to further reduce the risk of CARE Check vital signs, including temperature and level of con-sciousness, every 4 hours or more frequently as significant changes to the routine as-sessments provide information about the CLIENT s cardiovascularstatus and can give early indications of complications such as excessive bleeding, fluid volume deficit, and infection.
4 Perform neurovascular checks (color, temperature, pulses andcapillary refill, movement, and sensation) on the affected limbhourly for the first 12 to 24 hours, then every 2 to 4 abnormal findings to the physician can disrupt the blood supply to or innervation of the af-fected extremity. If so, rapid intervention is important to preservethe function of the extremity. Monitor incisional bleeding by emptying and recording suc-tion drainage every 4 hours and assessing the dressing blood loss can occur with a TOTAL JOINT re-placement, particularly a TOTAL hip replacement . Reinforce the dressing as dressing is usuallychanged 24 to 48 hours after surgery but may need reinforcementif excess bleeding occurs.
5 Maintain intravenous infusion and accurate intake and outputrecords during the initial postoperative CLIENT is atrisk for fluid volume deficit in the initial postoperative period be-cause of blood and fluid loss during surgery, as well as the effectsof the anesthetic. Maintain bed rest and prescribed position of the affected ex-tremity using a sling, abduction splint, brace, immobilizer, orother prescribed positioning of the affected ex-tremity is vital in the initial postoperative period so that the jointprosthesis does not become dislocated or displaced. Help the CLIENT shift position at least every 2 hours while on of position helps prevent pressure sores and othercomplications of immobility. Remind the CLIENT to use the incentive spirometer, to cough,and to breathe deeply at least every 2 measuresare important to prevent respiratory complications such aspneumonia.
6 Assess the CLIENT s level of comfort frequently. Maintain PCA,epidural infusion, or other prescribed analgesia to pain management promotes healing andmobility. Help the CLIENT get out of bed as soon as allowed. Teach and re-inforce the use of techniques to prevent weight bearing on theaffected extremity, such as the over-head trapeze, pivot turn-ing, and mobility prevents complications such aspneumonia and thromboembolism, but appropriate techniquesmust be used to prevent injury to the operative site. Initiate physical therapy and exercises as prescribed for thespecific JOINT replaced, such as quadriceps setting, leg raising,and passive and active range-of- motion exer-cises help prevent muscle atrophy and thromboembolism andstrengthen the muscles of the affected extremity so that it cansupport the prosthetic JOINT .
7 Use sequential compression devices or antiembolism stock-ings as help prevent thromboembolism andpulmonary embolus for the CLIENT who must remain immobilefollowing surgery. For the CLIENT with a TOTAL hip replacement , prevent hip flexionof greater than 90 degrees or adduction of the affected a seat riser for the toilet or measuresprevent dislocation of the JOINT . Assess the CLIENT with a TOTAL hip replacement for signs of pros-thesis dislocation, including pain in the affected hip or short-ening and internal rotation of the affected leg.(continued)1244 UNIT XI / Responses to Altered Musculoskeletal FunctionNURSING CAREOF THE CLIENT HAVING TOTAL JOINT replacement (continued) For the CLIENT with a TOTAL knee replacement , use a continuouspassive range-of- motion (CPM) device or range-of- motion exercises as is not a problem with a kneereplacement, and more emphasis is placed on range-of-motionexercises in the early postoperative period.
8 Maintain fluid intake and encourage a high-fiber stool softeners or rectal suppositories as contributes to the potential problem of constipation;these measures help maintain regular fecal elimination. Encourage consumption of a well-balanced diet with nutrition promotes tissue healing. Teach or reinforce postdischarge exercises and activity restric-tions. Emphasize the importance of scheduled follow-up physi-cian are discharged from the acute care facilitybefore healing is complete. Exercises are prescribed and activitiesare resumed gradually to protect the integrity of the JOINT replace-ment and prevent contractures. For those clients needing additional direct care after discharge,arrange placement in a long-term care or rehabilitation restrictions may preclude discharge to home for someclients.
9 Make referrals as needed to home health agencies and physi-cal often require home health care for both nurs-ing care needs and continued physical therapy following dis-charge from acute or long-term PromotionAlthough OA cannot be prevented, maintaining a normalweight and HAVING a program of regular, moderate exercise willreduce risk factors. Glucosamine and chrondroitin are popularnutritional supplements for OA that are increasingly popularand have been found to be of benefit in reducing manifesta-tions. clients should discuss these supplements with theirhealth care provider before using the following data through the health history and phys-ical examination (see Chapter 37). Health history: family history of OA, occupation, recre-ational activities, JOINT pain and stiffness, ability to carry outADLs and self-care activities Physical assessment: height/weight; gait, joints: symmetry,size, shape, color, appearance, temperature, pain, crepitus,range of motion , Heberden s nodes, Bouchard s nodesNursing Diagnoses and InterventionsChronic PainPain is a primary manifestation of OA.
10 As JOINT tissues degen-erate and changes in JOINT structure occur, the amount of dis-comfort generally increases. The pain associated with OA in-creases with activity and tends to be relieved with comfort measures are appropriate, withmild analgesics used to supplement these as needed. Monitor the CLIENT s level of pain, including intensity, loca-tion, quality, and aggravating and relieving factors. Accurateassessment of pain provides a basis for evaluation of the effect of interventions. Teach clients to take prescribed analgesic or anti-inflammatory medication as needed. Analgesics reduce theperception of pain and may decrease muscle spasm as medication may be ordered to decreaselocal inflammatory response in affected joints.