Transcription of Performing an A-G patient assessment: a step-by-step guide
1 Copyright EMAP Publishing 2020. This article is not for distribution except for journal club use Clinical Practice Keywords ABCDE/ assessment /. Deterioration/Goals Review assessment This article has been double-blind peer reviewed In this S. tep-by- step description of the A-G method of patient assessment Benefits of using A-G assessment in emergency and routine situations How to use A-G assessment in daily nursing practice Performing an A-G patient assessment : a step -by- step guide Key points Author Xabi Cathala is lecturer, School of Health and Social care /Institute of The A-G assessment Vocational Learning; Calvin Moorley is associate professor for nursing research and is a systematic diversity in care , School of Health and Social care /Adult nursing and Midwifery approach useful Studies; both at London South Bank University. in routine and emergency Abstract The A-G method is a systematic and structured approach of assessing situations patients , useful both in routine and emergency situations.
2 It is based on the ABCDE. approach used when resuscitation may be needed, extended by two additional steps. A-G stands for The ability to perform an A-G assessment is a key nursing skill, as it should be airway, breathing, standard practice not only in critically ill or deteriorating patients , but in all patients circulation, disability, receiving care . exposure, further information and Citation Cathala X, Moorley C (2020) Performing an A-G patient assessment : a goals practical step -by- step guide . nursing Times [online]; 116: 1, 53-55. N. This offers a systematic approach umerous assessments exist in (Resuscitation Council UK, 2015) and guid- to patient nursing . They are vital tools in ance from Benson (2017) on how to undertake assessments day-to-day practice. The A-G the F and G elements. Using this structured assessment is becoming a com- approach can ensure the reliability of the The ability to monly used tool in primary and secondary assessment in any situation.
3 An A-G assess- perform an A-G care settings. It integrates the procedure ment is not only used in critically ill or dete- assessment is a mandated for resuscitation and emergency riorating patients , but should be standard key nursing skill situations. However, it is also useful for practice for all patients receiving care . It nor- systematic baseline patient assessment mally takes a few minutes to complete Re-assessing and can improve patient mortality in hos- depending on the practitioner's experience. regularly will help pital (Griffiths et al, 2018). nurses detect A-G covers: airway, breathing, circula- Airway deterioration early tion, disability, exposure, further informa- The airway includes the nose, mouth, tion (including family and friends) and larynx, pharynx, trachea, bronchi and goals (Benson, 2017). Its systematic bronchioles (Cathala and Costa, 2019).
4 Its approach has been proven effective in iden- main function is to carry air into the body. tifying deteriorating patients or those at risk The aim of airway assessment is to ensure of deterioration (Dean and Bowden, 2017). this anatomical function is achieved and Nurses Performing the assessment any obstruction (full or partial) of the need to explain to the patient what they are airway is identified (Table 1). An indication going to do and seek their informed con- of a patent airway is the patient 's ability to sent. Before approaching the patient , they speak with a usual voice in full sentences. need to undertake a risk assessment of the environment to determine whether it is Breathing safe to undertake the A-G assessment . Breathing is the process by which air This article is based on the Resuscitation moves in and out of the lungs, allowing Council's approach to an A-E assessment gaseous exchange.
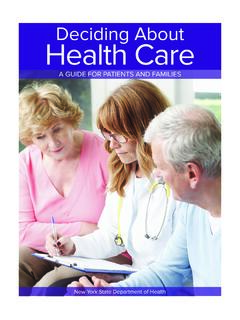
5 It should be: nursing Times [online] January 2020 / Vol 116 Issue 1 53 Copyright EMAP Publishing 2020. This article is not for distribution except for journal club use Clinical Practice Review hypercapnia (Williams, 2019; National present, monitor its output regularly, and Table 1. Main causes and signs Guideline Centre, 2010; National Institute ensure the patient has patent intravenous of airway obstruction for Health and care Excellence, 2018; access, so that fluids can be administered O'Driscoll et al, 2008). The patient 's ability in case of an emergency (Cathala and Main causes of airway obstruction to talk in full sentences is a good indicator Moorley, 2018) (see Box 2). In healthcare settings, compromised of their breathing status. airway is often a result of altered level Listening to the breathing sounds can Disability of consciousness give an idea of the cause of any breathing Disability assessment focuses on the main F oreign body, aspiration difficulty.
6 Rattling noises can indicate causes of reduced consciousness such as Laryngotracheal trauma secretion, wheezing can infer asthma, fainting (falls and mobility), drugs (polyp- Vocal cord paralysis while stridor can suggest partial airway harmacy and side effects), alcohol, poisons Allergic reaction obstruction (Cathala and Costa, 2019). and hypoglycaemia. The patient 's ACVPU. Laryngeal oedema Placing both hands on the patient 's chest status should be assessed. ACPVU stands Oedema to feel for the rise and fall that accompany for alert, confusion (new), response to Haematoma breathing will help nurses assess chest voice, painful stimuli, and unconscious Abscess expansion and determine symmetry between (Smith et al, 2017). Signs of partial airway obstruction the right and left lungs. Consent need to be Other areas of the assessment include obtained from the patient and a chaperone the pupillary size and reaction to light: Breathing sounds (gurgling, stridor, should be offered where indicated.)
7 Pupils should be of equal size and shape bubbling, expiratory wheeze). A more accurate assessment is an aus- and reactive to light. Nurses also need to Choking cultation with stethoscope, but this check the medication chart looking for any Gasping for air requires advanced skills. drug-induced effects. Laboured breathing (possibly noisy). Measuring blood glucose is an important Coughing Reduced level of consciousness Circulation part of disability assessment . Hypoglycaemia Assessing circulation is not limited to an (blood glucose < ) can reduce the Unable to speak in full sentences assessment of the heart. It is focused on patient 's consciousness level (Kitsuta, 2006). Use of accessory muscles in breathing the haemodynamic and vascular parts of and needs to be treated following local trust Signs of complete airway obstruction the circulatory system.
8 Policies and guidelines. Clinical judgement Agitation This assessment starts with the periph- should be used if the patient is not diabetic;. patient unable to speak eries. Are the hands and fingers blue, pink, blood glucose levels may not need to be Difficulty breathing pale, warm, cold? Blue, pale and cold can checked but if there are signs of altered levels No air entry at the auscultation reflect a poor peripheral circulation, while of consciousness (Box 3) then the blood glu- (no chest movement, or see-saw' pink and warm are linked with a good cose level should be measured. Measuring breathing) peripheral circulation. arterial or venous blood gas can be helpful in Gasping for air Another useful measure is capillary such situations. In diabetic patients with Choking refill time (CRT). A CRT <2 seconds sug- high blood sugar levels, it is important to Panic gests a good peripheral perfusion (Sansone look for signs of ketoacidosis (Box 3).)
9 Cyanosis (late sign) et al, 2017). High-pitched breathing noises The next part of the assessment is the Box 1. Respiratory warning (wheezing) heart rate, taking the peripheral or central signs Unconsciousness pulse. Assessing the pulse involves deter- Stridor mining its presence, regularity, quality and l Respiratory distress signs: sweating, volume for 15 seconds. The rate is assessed central cyanosis, use of accessory l E. ffortless; for one full minute. An acceptable heart rate respiratory muscles (abdominal l E. qual bilateral chest expansion; should be between 51 and 90 beats per minute breathing, see-saw' breathing). l A t a rate of 12-20 breaths per minute (Royal College of Physicians, 2017). The pulse l Respiratory rate <12bpm or >20bpm (respiratory rate); should be regular and strong or bounding. l Oxygen saturations outside the l N oise-free; that is, no wheezing, stridor An acceptable systolic blood pressure is normal values, which are: (a harsh vibrating noise) or rattling; between 111 and 219 mmHg (Royal College of l >96% for patients without l The airway should be free of sputum.
10 Physicians, 2017). Clinical readings should hypercapnic respiratory failure or During the assessment , nurses must be interpreted with caution. If the systolic with chronic obstructive use the Look, Listen and Feel technique. blood pressure differs by 10mmHg from pulmonary disease (COPD). Looking for any respiratory distress signs the patient 's baseline, the result should be l 88-92% for patients with (Box 1), assessing the depth and pattern of reviewed with another member of the team. hypercapnic respiratory failure the respiratory cycle for 15 seconds and Although diastolic blood pressure is not or with chronic obstructive counting the respiratory rate for a full part of the NEWS 2 scoring system a reading pulmonary disease (COPD) or at minute is recommended The acceptable it will give a good indication of the patient 's risk of worsening hypercapnia oxygen saturation is >96% for patients haemodynamic status.