Transcription of Postmenopausal Pharmacotherapy Newsletter
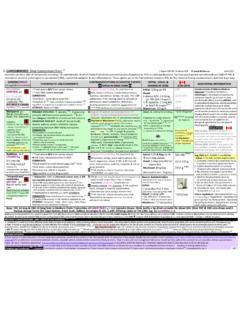
1 POSTMENOPAUSALPHARMACOTHERAPYS eptember, 1999As Canada's baby boomers age, more and more women will facethe option of Hormone Replacement Therapy (HRT). Thedecision can be a difficult one given the conflicting pros and RxFiles examines the role and use of HRT, as well as newerSERMS and bisphosphonates in post-menopausal (PM) is indicated for the treatment of PM symptoms such asvasomotor disturbances and urogenital atrophy, and is consideredprimary therapy for prevention and treatment of postmenopausalosteoporosis (PMO).1 Contraindications are reviewed in Table HRT is contraindicated in women with active breast oruterine cancer, note that a prior or positive family history of thesedoes not necessarily preclude women from receiving Replacement Therapy (ERT)Naturally secreted estrogens include:2westrone (E1): acts as natural reservoir for E2 with which it easilyintraconverts in vivo.
2 The main estrogen after menopausewestradiol (E2): the predominant, most potent, and physiologicallyimportant estrogen produced by the ovary in the reproductive yearswestriol (E3): a metabolite of E1 and E2 Estrogens cause proliferation of breast tissue and vaginal anduterine mucosa, inhibit rate of bone resorption, and have positiveeffects on skin, the cardiovasculature, immune system, and interactions may be seen with anticoagulants, hypoglycemics,antihypertensives and drugs that affect the CYP450 enzyme Efficacy: The most common estrogens prescribed forHRT are the conjugated estrogens containing primarily estrone andequilin from either equine urine (CEE, Premarin ) or plantsources (CES ). Estradiol, also from plant sources, is contained inmany of the other oral and topical products. Regardless of theirsource, equivalent doses of oral estrogen products produce similarestradiol/estrone plasma levels because of rapid conversion tothese forms in There is no objective data to suggest anyproduct is more efficacious than others.
3 All are effective in theshort-term management of PM symptoms. Long-term therapy isbeneficial in preventing PMO and possibly Alzheimer's. In somecases, lower-dose ERT ( CEE po daily) given withcalcium supplements may also prevent of ,5 Cardiovascular benefits have also been demonstrated6; however,due to a lack of benefit in patients with existing coronary heartdisease (CHD) in the HERS trial, HRT is not currentlyrecommended for the secondary prevention of ,8,1 Severallarge-scale, long-term prospective studies are best route of administration depends on indication and patientpreference. Transdermal therapy is preferred in women unable totake oral products due to intolerance or contraindications such asliver dysfunction or elevated triglycerides. Local vaginal therapiesin the form of creams or a vaginal ring (Estring ) are effective forurogenital PM symptoms.
4 They have variable, dose-relatedsystemic absorption (levels up to 25% of equivalent oral dosing).HIGHLIGHTS wwwwLong term HRT carries several major benefits but also riskswhich should be evaluated on an individual and ongoing basiswwwwContinuous ERT is appropriate for women without a uteruswwwwWomen with a uterus should receive progestagen (at least 12days per month or continuous low-dose) as part of their HRTwwwwLow-dose ERT (CEE ) + Ca++ appears to prevent PMOwwwwBisphosphinates ( alendronate, etidronate) and raloxifene arealternatives to HRT in treating and preventing PMOwwww"Natural" HRT regimens can be compounded but data is lackingComparative Safety: Because of differences between products,some side effects may be alleviated by switching from one productto another, particularly from equine to plant sources or from oral totopical (see Table 3 - Side Effects & Their Management).
5 Unopposed oral or transdermal ERT increases the risk ofendometrial hyperplasia and uterine cancer. Women with an intactuterus must receive progestagen therapy either sequentially orcontinuously to minimize this risk. Despite its many benefits, longterm ERT also carries an increased risk of breast cancer of 2% peryear of use over 5 Addition of progestagen does not appearto protect against this risk. (See Table 4- Risks vs. Benefits)Progestagen Replacement Therapy (PRT)Naturally occurring progesterone transforms an estrogen-primedproliferative endometrium into a secretory endometrium. PRT isindicated to prevent the endometrial hyperplasia caused byunopposed estrogen therapy in women with intact uteri. Availableprogestagens include the natural plant-derived progesterone(Prometrium ) and the synthetic progestins, medroxyprogesteroneacetate (MPA/Provera ) and norethindrone (in Estracomb patch).
6 Comparative Efficacy: Oral progestagens are effective inpreventing endometrial hyperplasia but do not reduce the long termrisk of breast cancer with HRT. Although synthetic progestinsseem to attenuate the beneficial lipid effects of estrogens ( HDL-C), combination HRT appears to confer the same cardioprotectiveeffect as Safety: Side effects are more problematic with thesynthetic progestins, higher dose PRT, and sequential therapy(Table 3). Sedation is more prevalent with Prometrium whichmay require dividing the dose and/or administration at derivatives (norethindrone) tend to produce more androgenicside effects and greater lowering of HDL-C than ReplacementWomen who have undergone oophorectomy may require androgentherapy. Decreased libido and loss of energy or sense of well-being may be caused by androgen deficiency and requiresupplementation.
7 Data is limited as to optimal injection contains testosterone enanthate incombination with estradiol dienanthate. Climacteron can be given IM every 4-6 weeks. If a larger estrogencomponent is desired, Delestrogen injection may be addedto the same syringe. The recent SOGC consensus stated that 1mldose of Climacteron used in the past should be avoided due to theproblems of hirsutism, virilization, and long term testosterone undecanoate (Andriol ) 40mg EOD is mostcommonly used but data is lacking. Vaginal ointments of eithertestosterone propionate1 or micronized testosterone11 can becompounded in select pharmacies, although data is is partly metabolized to estrogen and thus womenwith an intact uterus will require progestagen opposition. Womentaking androgens should be monitored for potential adverse effectson lipids and symptoms of androgen excess (hirsutism, voicechanges, and clitoromegaly).
8 SELECTING AN HRT REGIMENC onsiderations: Although many women would benefit fromHRT12, only 15-25% of eligible women avail themselves of is poor, estimated at <30%. Of 1st time users, 20-30%will never fill their script, 20% will discontinue therapy within 9months, and 10% will take their pills Commonreasons for refusing HRT include side effects, non-acceptance ofbleeding, complicated regimens, and fear of Patienteducation and careful individualization of therapy can significantlyboost compliance with hysterectomies may receive unopposed ERT asaddition of progesterone is not required to protect the ERT is now recommended as cyclic regimens ( 1-25) often resulted in the uncomfortable return ofmenopausal symptoms in the withdrawal with intact uteri should receive continuous estrogencombined with a progestagen to prevent endometrial progestagen may be given either sequentially for a minimumof 12-14 days per month or continuously.
9 Common regimens arecompared in Table 1."Natural" or "Bioidentical" HRT is an evolving alternativeapproach to HRT which attempts to mimic the physiologicalpattern of estrogens (E1,E2,E3), progesterone, and preparations are not available thus requiringcompounding of products ( Tri-est cream, progesterone cream)at select pharmacies. Many questions remain as data on efficacyand safety is There is no evidence that percutaneousprogesterone creams offer protection against endometrial estrogen receptor modulators (SERMs) have recentlybeen developed in an attempt to gain the skeletal andcardioprotective benefits of the estrogens without increasing therisk of breast or endometrial cancer. Raloxifene (Evista ) 60mgdaily is indicated for the prevention of PMO. Bone density ismaintained or slightly increased in both the spine and the data also shows a reduction in vertebral, but notnonvertebral fractures, after one It also lowers LDLcholesterol.
10 Raloxifene does not stimulate uterine or breast tissue,and may even reduce the risk of breast Disadvantagesinclude its high cost relative to HRT, a risk of thromboembolismsimilar to ERT, and its lack of benefit in relieving MP symptomswhich may actually worsen in some are the most effective agents to reduce bone are valuable agents in preventing PMO when HRT isotherwise not indicated or undesirable. Cyclic etidronate andcalcium ( Didrocal ) and alendronate (Fosamax ) 10mg areindicated for treatment of osteroporosis. Low-dose alendronate(5mg daily) has recently been approved for the prevention of maintains bone mass in more than 85% of treated women whenstarted within 5 years of In Saskatchewan, only the 10mgalendronate currently has drug plan (EDS) AGENTSC alcium and Vitamin D is essential in preventing PMO. It isrecommended that PM women get at least 1,000 mg (1,500 mg ifnot on HRT) of calcium and 400-800 IU of Vitamin D per carbonate is a preferred form and a variety of supplementsare available ( TUMs , Apo -Cal).