Transcription of Provider Appeal Form - bcidaho.com
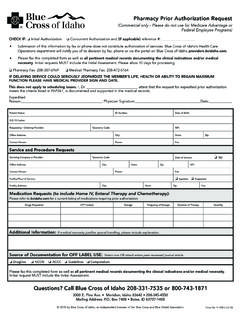
1 2021 by Blue Cross of Idaho, an independent licensee of the Blue Cross and Blue Shield AssociationForm (10-21)Submit separate forms and Appeal documentation when submitting appeals for multiple providers and/or members. Please include all of the pages of this form in your : Inquiry Information:All Provider inquiries should be submitted as a post-service claim reconsideration through the Provider portal at See PAP236, MAPAP229, HCBSPAP225 and form is to be used only for first- or second-level appeals after you have exhausted all resolution efforts through the online post-service claim inquiry include the email contact number assigned in your initial inquiry response. Contact #: Please also include your Prior Authorization Reference number if applicable.
2 Reference #: This form should only be used for reasons documented in your Provider contract, such as: Medical Necessity Investigational Clinical Editing Prior Authorization Application of the Maximum AllowanceLevel of Appeal (Required): First-Level Appeal Second-Level of Appeal (review your contract for associated costs)Important Information:Are you a contracting Provider with Blue Cross of Idaho? Yes NoAre the charges in question Provider liability? Yes NoIf you answered No to either of the above two questions and intend to Appeal on behalf of the member, a completed Authorized Representative Form for commercial lines of business or a Waiver of Liability Form for government lines of business must be included with the Appeal documentation. Provider Appeal Form 2021 by Blue Cross of Idaho, an independent licensee of the Blue Cross and Blue Shield AssociationProvider Information: Provider or facility nameProvider ContactAddressCity/StateZip codeProvider email (Required)Phone numberFax numberNPITax ID #Member Information:First nameLast nameDate of birth (MM/DD/YYYY)Member ID prefix, number and suffix Group numberClaim Information:Date of service (MM/DD/YYYY)Claim numberTotal chargeReasons for Appeal and Documentation Needs: Medical Necessity Include rationale, medical record documentation and criteria to support medical necessity.
3 Investigational Blue Cross of Idaho considers, at its discretion, current published medical literature and peer-review publications based on scientific evidence, and evidence-based guidelines developed by national organizations and recognized authorities. Clinical Editing For reconsideration of the application of clinical editing, please submit documentation or literature from a nationally recognized organization such as national correct coding initiative (NCCI). Application of the Maximum Allowance Specify code in question, expected allowance and include a detailed explanation and documentation supporting your request for review. Prior Authorization, compelling reasons may include: Evidence that member presented with incorrect insurance information Member was unable to communicate and individuals in attendance are unable to provide coverage information Evidence that the Provider attempted to submit an inpatient notification or prior authorization following Blue Cross of Idaho policy Approved authorization on file yet the claim denied Evidence that the need for an authorization could not be anticipated prior to the service being renderedProvider Appeal FormForm (10-21) 2021 by Blue Cross of Idaho, an independent licensee of the Blue Cross and Blue Shield AssociationProvider Appeal FormAdditional Information (Provide Explanation or Attach Letter):Submission Information:Note.
4 To ensure receipt and streamline processes, please combine all documents into one attachment when submitting your Appeal by : 208-286-3559 Email: confidential Request Blue Cross of Idaho Attn: Provider Resolutions Box 7408 Boise, ID 83707 Form (10-21)