Transcription of SIGN 128 • The SIGN discharge document
1 sign 128 The sign discharge document June 2012 ImprovementHelp us to improve sign guidelines -click here to complete our survey This document is produced from elemental chlorine-free material and is sourced from sustainable Intercollegiate Guidelines NetworkThe sign discharge documentJune 2012 The sign discharge documentScottish Intercollegiate Guidelines Network Elliott House, 8 -10 Hillside Crescent Edinburgh EH7 5EA published June 2012 ISBN 978 1 905813 89 6 Citation textScottish Intercollegiate Guidelines Network ( sign ). The sign discharge document . Edinburgh: sign ; 2012. ( sign publication no. 128). [June 2012]. Available from URL: consents to the photocopying of this guideline for the purpose of implementation in sign discharge documentContents1 Introduction .. The need for a sign discharge document .. Remit of the sign discharge document .
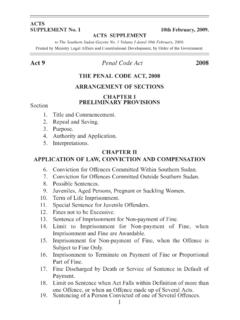
2 12 The discharge document .. The content of the discharge document .. Use of the discharge document ..33 The sign discharge document template ..54 Implementing the sign discharge document .. Implementation strategy ..105 Development of the sign discharge document .. The sign discharge document development Consultation and peer review ..12 Abbreviations ..15 sign discharge documentThe sign discharge documentThe sign discharge documentThe sign discharge document1 THE NEED foR A sign discharge DoCumENTThe preparation and sharing of accurate and timely records of care and treatment are central aspects of good clinical practice and the principles of good medical practice set out by the General Medical Council (GMC)1 will therefore apply in the provision of discharge who are discharged from hospital will be discharged back into the care of the general practitioner (GP) with whom they are registered.
3 Essential information about the patient s stay in hospital that allows the GP to continue the patient s care and management following their discharge from hospital is sent by the hospital to the patient s GP in the form of a discharge document (DD). There are currently two forms of DD in use: the Immediate discharge document (IDD), which should be sent to the GP on the day of discharge , and a discharge summary or letter, which contains more detailed information about the patient s stay in hospital and is sent out, ideally, within a week of the patient s discharge date. The content, structure and production (particularly the timeliness) of discharge documents have long been a cause for concern and in order to try to address these issues, a minimum dataset for the IDD was published by sign in 1996 ( sign 5)2 and revised and updated by sign in 2003 ( sign 65).3 Improving the quality and timeliness of discharge documents may lead to improvements in patient safety by improving the process of transition from hospital to GP THE NEED FoR AN UPDATEThis sign DD replaces sign 65 and reflects a number of developments including advances that have been made with regard to the production, use and transmission of electronic documents within NHSS cotland, changes in terminology, and the importance of medicines reconciliation.
4 sign 5 and sign 65 reflected the fact that many discharge documents were still produced and/or printed on paper and transmitted by post, hand or fax. This update reflects the fact that the production and communication of documents by electronic means within both primary and secondary care is becoming more these developments, the essential components of a DD remain largely unchanged with the content, quality and accuracy of the information contained in the DD and timely transmission to the GP being the key REmIT of THE sign discharge ovERALL oBJECTIvESThe aim of this document is to present a template for a single discharge document that can be used as both the IDD (in its core format) for every patient on the day of discharge , and as the final discharge summary/letter (in its extended format) for more complex sign DD is designed for patients who are discharged from hospital following an inpatient stay, ie, a stay in hospital of one night or more.
5 It could also, however, form the basis of a DD for patients receiving treatment on a day-case sign IDD is not designed to cover discharges from psychiatric care because of the special information needs relating to this group of patients, but it could form the basis of a DD tailored to the needs of this sign DD is effectively a minimum dataset. As such the template should not limit the information provided and, where necessary, additional information relating to, for example, anticipatory care planning, should be provided either in the DD or separately, as appropriate.| 1 IntroductionThe sign discharge TARGET USERS oF THE sign DICHARGE DoCUMENTThe sign DD is of relevance to all hospital medical and nursing staff, allied health professionals, general practitioners, community nurses, pharmacists, and out-of-hours sign DD is not intended to be the sole or main source of information for patients, their carers or relatives, although most will receive a copy at the time of discharge from |The sign discharge document2 The discharge THE C oNTENT of THE discharge DoCumENTSIGN 5 argued the importance of a minimum dataset as a basis for electronic data transfer and specified such a dataset; sign 652 refined the original dataset to encourage improvements in the standard of discharge documents in this critical area of practice.
6 It was recognised in sign 65 that a minimum dataset should be evidence based and include all those items seen as sign DD is based on a review of sign 65 by a multidisciplinary group (see section ) using an amended version of the sign guideline development process (see sections and ). The content, although similar to sign 65, has been revised and updated; some existing items have been deleted or changed, new items have been added and the guidance notes have been reviewed and uSE of THE discharge DoCumENTThe sign DD is a single discharge document template, with core and extended formats, for use within core discharge document (CDD), which replaces the IDD, must be produced for all patients on the day of discharge . In cases where the patient s stay in hospital is brief and uncomplicated and where there are no outstanding test results or investigations, the CDD will be the sole discharge more complex cases where more detailed information about the hospital stay or follow-up arrangements is required, or where the results of tests and investigations are awaited, an extended discharge document (EDD) will also have to be completed.
7 In cases where an EDD is required, the CDD, which will be retained on the hospital information system, can be extended and augmented by the addition of more detailed information in specified fields to produce the EDD. When an EDD is produced it is important, for audit purposes, that the CDD is retained on the system EDD should be sent out within seven days of the date of discharge to ensure that the GP has all the information required for the ongoing care and management of the patient. In cases where important information, such as test results, is not available within seven days, dispatch of the EDD can be delayed until the information is available but this delay should not exceed 14 relevant members of the multidisciplinary hospital team should be involved in the production of the CDD and the EDD. The facility to automatically transfer information from nursing, pharmacy, physiotherapy, occupational therapy and other relevant records would greatly facilitate this CoDING oF DIAGNoSES, oPERATIoNS AND PRoCEDURESA ccurate reporting of all diagnoses, operations and procedures relevant to a patient s admission is an essential part of both the CDD and the EDD.
8 This information is central to the future care and management of the patient and essential for accurate coding and record keeping within hospital and general practice records systems. Clear textual descriptions of these items must therefore be addition to textual descriptions, both the CDD and the EDD ask for standard codes to be provided for these items where possible. However, there is currently no national definition of standard codes across NHSS cotland with hospitals tending to use the International Statistical Classification of Diseases and Health-related Problems, tenth revision (ICD-10) and the office of Population Censuses and Surveys Classification of Surgical operations, fourth revision (oPCS-4) and general practices tending to use Read codes. Although the adoption of a single coding system (eg the Systemised Nomenclature of Medicine - Clinical Terms (SNoMED-CT) across NHSS cotland would greatly facilitate the transfer of information between, for example, hospitals and general practices, until such a system is agreed the definition of what constitutes a standard code will be a matter for local agreement.)
9 The extent to which standard codes are included in the CDD and EDD will also depend on local systems and processes.| 3 The discharge documentThe sign discharge MEDICINES RECoNCILIATIoN AT DISCHARGEThe accurate recording of medicines is an essential component of the CDD and EDD as it has a direct impact on patient care and management and is an important factor in improving patient safety. In the context of both the CDD and EDD, medicines reconciliation comprises the accurate recording and comparison of all medicines a patient was taking on admission to hospital with those they are taking at the time of discharge from hospital, documenting all changes that have taken place. Changes can include the prescription of new medicines, changes to existing medicines (such as changes to dose or frequency) and the stopping of medicines that the patient was taking at the time of admission to reflect the importance of including accurate information on all new, continuing and stopped medicines, the sign DD now includes separate and extended sections for recording this information along with more detailed guidance notes for the discharge document with the patient s community pharmacist is considered to be an important step in improving medicines reconciliation at discharge and enhancing patient safety relating to medicines.
10 The decision to share the DD with the community pharmacy must, however, be made in accordance with local CoNSULTANT sign -oFFIn cases where the CDD is the sole discharge document it must be signed off by the consultant or senior doctor who is responsible for coordinating the care of the patient at the time of discharge . If consultant or senior doctor sign -off is not possible at the time of discharge , an unsigned copy of the CDD should be sent on the day of discharge followed by a signed copy within seven days of cases where the CDD is to be followed by an EDD, the CDD does not have to be signed by the consultant or senior doctor coordinating the care of the patient, although it is good practice to do so whenever EDD must always be signed by the consultant or senior doctor responsible for coordinating the care of the patient at the time of definition of senior doctor will be a matter for local |The sign discharge document3 The sign discharge document templateItemfieldsNotesItems shown in bold are essential for the core and extended discharge not in bold are desirable for the extended discharge core discharge document (CDD)