Transcription of The Management of Diabetic Ketoacidosis in Adults
1 Supporting, Improving, CaringJoint British Diabetes SocietiesInpatient Care Group The Management of DiabeticKetoacidosis in AdultsMarch 2010 Writing GroupMark W Savage (Chair of Sub Group) Maggie Sinclair-Hammersley (Chair of JBDS IP Care Group) Gerry Rayman Hamish CourtneyKetan DhatariyaPhilip Dyer Julie Edge Philip Evans Michelle Greenwood Girly HallahanLouise Hilton Anne KilvertAlan Rees and many othersGroups represented:Association of British Clinical Diabetologists; British Society ofPaediatric Endocrinology and Diabetes and Association of Children s Diabetes Clinicians;Diabetes Inpatient Specialist Nurse (DISN) Group; Diabetes UK; NHS Diabetes (England);Northern Irish Diabetologists; Society of Acute Medicine; Welsh Endocrine and DiabetesSociety; Scottish Diabetes Group. JBDS IP Group gratefully acknowledges the funding and administrative supportfrom NHS DiabetesBritish Society of Paediatric Endocrinology and Diabetes (BSPED) guidelines formanagement of DKA in young people under the age of 18 years can be found at: 3 PageForeword4 Introduction5 Rationale for Best Practice6 Controversial Areas8 Serious Complications of DKA or its treatment10 DKA Pathway of Care11 Implementation and Audit16 References17 Appendices201.
2 Conversion to subcutaneous insulin2. Joint British Societies Audit StandardsAppendix to followIntegrated Care PathwayContents4 Diabetic Ketoacidosis (DKA) though preventable remains a frequent and life threatening complication oftype 1 diabetes. Unfortunately, errors in its Management are not uncommon and importantly areassociated with significant morbidity and mortality. Most acute hospitals have guidelines for themanagement of DKA but it is not unusual to find these out of date and at variance to those of otherhospitals. Even when specific hospital guidelines are available audits have shown that adherence to andindeed the use of these is variable amongst the admitting teams. These teams infrequently refer early tothe diabetes specialist team and it is not uncommon for the most junior member of the admitting team,who is least likely to be aware of the hospital guidance, to be given responsibility for the initialmanagement of this complex and challenging address these issues the Joint British Diabetes Societies, supported by NHS Diabetes has produced up-to-date guidance developed by a multidisciplinary group of practicing specialists, with considerableexperience in this area.
3 Where possible the guidance is evidenced based but also draws from accumulatedprofessional experience. A number of new recommendations have been introduced including the use ofbedside ketone meters (though Management based on bicarbonate and glucose are retained for those yetto introduce ketone meters), the use of fixed rate intravenous insulin infusion , and mandatory and promptreferral to the diabetes specialist team in all cases. The Management is clearly presented and divided into anumber of key steps in the care pathway; the first hour, the next six hours, next twelve hours , conversion to subcutaneous insulin and preparing for discharge home are included. Audit isencouraged against defined guideline is clearly written and accompanied by a practical and easy to follow flow chart to be used inadmitting departments and wards managing authors should be congratulated on their achievement. These guidelines are recommended to alldiabetes hospital teams for rapid introduction and for acceptance as the national guideline for managingDKA.
4 Their widespread introduction should significantly improve the care of people admitted with G RaymanNHS Diabetes Clinical Lead for Inpatient Diabetes CareForeword5 There are several currently available national andinternational guidelines for the Management ofDiabetic Ketoacidosis (DKA) in both Adults andchildren. (ISPAD 2009, McGeoch 2007, Savage 2006,BSPED 2004, Kitabchi 2009). In the last decade,however, there has been a change in the way patientswith DKA present clinically and in addition there hasbeen rapid development of near-patient testingtechnology. Until recently there was no easilyavailable assay for ketone bodies hence capillaryglucose, venous pH and bicarbonate were used todiagnose and monitor response to treatment in patient testing for 3-beta-hydroxybutyrate isnow readily available for the monitoring of theabnormal metabolite allowing for a shift away fromusing glucose levels to drive treatment decisions inthe Management of DKA. These guidelines have beendeveloped to reflect the development in technologyand reflect new practice in the UK.
5 They are evidencebased where possible but are also drawn fromaccumulated professional knowledge and consensusagreement. They are intended for use by any healthcare professional that manages DKA in Ketoacidosis (DKA) is a complex disorderedmetabolic state characterised by hyperglycaemia,acidosis, and ketonaemia. DKA usually occurs as aconsequence of absolute or relative insulin deficiencythat is accompanied by an increase in counter-regulatory hormones (ie, glucagon, cortisol, growthhormone, epinephrine). This type of hormonalimbalance enhances hepatic gluconeogenesis andglycogenolysis resulting in severe lipolysis increases serum free fatty acidsthat are then metabolised as an alternative energysource in the process of ketogenesis. This results inaccumulation of large quantities of ketone bodiesand subsequent metabolic acidosis. Ketones includeacetone, 3-beta-hydroxybutyrate, and predominant ketone in DKA is are several mechanisms responsible for fluiddepletion in DKA. These include osmotic diuresis dueto hyperglycaemia, vomiting commonly associatedwith DKA, and eventually, inability to take in fluid dueto a diminished level of consciousness.
6 Electrolyteshifts and depletion are in part related to the osmoticdiuresis. Hyper and hypokalaemia need and DiagnosisDKA consists of the biochemical triad of ketonaemia,hyperglycaemia, and true incidence is difficult to establish. Population-based studies range from to 8 episodes per 1,000patients with diabetes (Johnson 1980, Faich 1983).DKA remains a significant clinical problem in spite ofimprovements in diabetes care (Fishbein 1995,Umpierrez 19997).Mortality and MorbidityImproved understanding of the pathophysiology ofDKA with close monitoring and correction ofelectrolytes has resulted in a significant reduction inthe overall mortality rate from this life-threateningcondition. Mortality rates have fallen significantly inthe last 20 years from to (Lin 2005).The mortality rate is still high in developing countriesand among non hospitalised patients (Otieno 2005).This high mortality rate illustrates the necessity ofearly diagnosis and the implementation of effectiveprevention oedema remains the most common cause ofmortality, particularly in young children andadolescents.
7 The main causes of mortality in the adultpopulation include severe hypokalaemia, adultrespiratory distress syndrome, and co-morbid statessuch as pneumonia, acute myocardial infarction andsepsis (Hamblin 1989).IntroductionKetonaemia 3 mmol/L and over orsignificant ketonuria (more than 2+ on standard urine sticks)Blood glucose over 11 mmol/L or known diabetes mellitusBicarbonate (HCO3-) below 15 mmol/L and/orvenous pH less than and AcidosisUntil recently, Management of DKA has focussed onlowering the elevated blood glucose with fluids andinsulin, using arterial pH and serum bicarbonate toassess metabolic improvement. This is based on theassumption that this would efficiently suppressketogenesis and reverse acidosis. This strategyrecognised that blood glucose is only a surrogate forthe underlying metabolic abnormality. Recentdevelopments now allow us to focus on theunderlying metabolic abnormality (ketonaemia)which simplifies treatment of those who present withmodest elevation of blood glucose but with acidosissecondary to ketonaemia euglycaemic diabeticketoacidosis (Munro 1973, Johnson 1980, Jenkins1993).
8 This clinical presentation is being encounteredmore frequently. Improved patient education withincreased blood glucose and ketone monitoring hasled to partial treatment of DKA prior to admissionwith consequent lower blood glucose levels atpresentation. Bedside MonitoringThese guidelines recommend that Management isbased on bedside monitoring of patients with glucose is routinely checked at the bedside, butportable ketone meters now also allow bedsidemeasurement of blood ketones (3-beta-hydroxybutyrate). This is an important advance in themanagement of DKA (Sheikh-Ali 2008, Bektas 2004,Khan 2004, Wallace 2004, Vaneli 2003, Naunheim2006). The resolution of DKA depends upon thesuppression of ketonaemia, therefore measurementof blood ketones now represents best practice inmonitoring the response to treatment (Wiggam1997).Access to blood gas and blood electrolytemeasurement is now relatively easy and availablewithin a few minutes of blood being taken. Thereforeglucose, ketones and electrolytes, includingbicarbonate and venous pH should be assessed at ornear the bedside.
9 This recommendation raises important issues: Staff must be trained in the use of blood glucoseand ketone meters The meters should be subject to rigorous qualityassurance Laboratory measurement will be required in certaincircumstances, such as when blood glucose orketone meters are out of range .It is recognised that not all units have access toketone meters. Thus, guidance is also given onmonitoring treatment using of the rate of rise ofbicarbonate and fall in blood glucose as Involvement of Diabetes SpecialistTeams (DST)The diabetes specialist team must always be involvedin the care of those admitted to hospital with involvement shortens patient stay and improvessafety (Levetan 1995, Cavan 2001, Davies 2001,Sampson 2006). This should occur as soon aspossible during the acute phase but will depend onlocal circumstances. Specialists must also be involvedin the assessment of the precipitating cause of DKA, Management , discharge, and follow up. This willinclude assessment of the patient s understanding ofdiabetes plus their attitudes and beliefs.
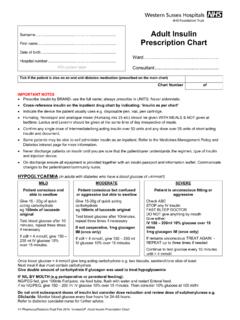
10 Specialistinvolvement is essential to ensure regular audit andcontinuous quality improvement in theimplementation of DKA guidelines. The practice ofadmitting, treating and discharging patients withDKA without the involvement of the diabetesspecialist team is unsafe and likely to compromisesafe patient care. This is a governance issue (Clement 2004).Recommended changes in Management Measurement of blood ketones, venous (notarterial) pH and bicarbonate and their use astreatment markers Monitoring of ketones and glucose using bedsidemeters when available and operating within theirquality assurance range Replacing sliding scale insulin with weight-basedfixed rate intravenous insulin infusion (IVII)Rationale for Best Practice - The New Paradigm7 Use of venous blood rather than arterial blood inblood gas analysers Monitoring of electrolytes on the blood gasanalyser with intermittent laboratory confirmation Continuation of long acting insulin analogues(Lantus or Levemir ) as normal Involvement diabetes specialist team as soon aspossibleGeneral Management IssuesFluid administration and deficitsThere is universal agreement that the most importantinitial therapeutic intervention in DKA is appropriatefluid replacement followed by insulin main aims for fluid replacement are.