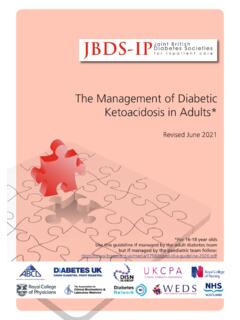
Transcription of The Management of Diabetic Ketoacidosis in Adults
1 The Management of Diabetic Ketoacidosis in Adults Where individuals aged 16-18 are managed by paediatric teams, the paediatric guidelines should be followed: Diagnostic criteria: all three of the following must be present BOX 3: 60 minutes to 6 hours Aims of treatment: BOX 5: 12 to 24 HOURS. capillary blood glucose above 11 mmol/L Rate of fall of ketones of at least mmol/L/hr OR bicarbonate rise 3. Expectation: By 24 hours the ketonaemia and acidosis should have capillary ketones above 3 mmol/L or urine ketones ++ or more mmol/L/hr and blood glucose fall 3 mmol/L/hr resolved. Request senior review is not improving Maintain serum potassium in normal range venous pH less than and/or bicarbonate less than 15 mmol/L Avoid hypoglycaemia Aim: Ensure that clinical and biochemical parameters are continuing to Action 1: Re-assess patient, monitor vital signs improve or are normal BOX 1: Immediate Management .
2 Time 0 to 60 minutes Hourly blood glucose (lab blood glucose if meter reading HI') Continue IV fluid replacement if not eating and drinking Hourly blood ketones if meter available If ketonaemia has cleared and the person is not eating or drinking, (T=0 at time intravenous fluids are commenced) Venous blood gas for pH, bicarbonate and potassium at 60 minutes, 2 move to a variable rate intravenous insulin infusion (VRIII) as per hours and 2 hourly thereafter local guidelines If intravenous access cannot be obtained request critical care support immediately Reassess for complications of treatment, fluid overload, cerebral Action 4: Further investigations If potassium is outside normal range, re-assess potassium replacement oedema Action 1: Commence sodium chloride solution (use a Capillary and laboratory glucose and checkhourly.)
3 If abnormal after further hour seek immediate senior Continue to treat precipitating factors large bore cannula) via an infusion pump Venous BG medical advice Transfer to subcutaneous insulin if the person is eating and drinking See Box 2 for rate of fluid replacement U&E and FBC Action 2: Continue fluid replacement via infusion pump as follows: normally and biochemistry is normal Action 2: Commence a fixed rate intravenous insulin infusion Blood cultures sodium chloride 1L with potassium chloride over next 2 hours Action 1 Re-assess patient, monitor vital signs (FRIII). ( based on estimate of weight) 50 ECG sodium chloride 1L with potassium chloride over next 2 hours Action 2 Review biochemical and metabolic parameters units human soluble insulin (Actrapid or Humulin S ) CXR sodium chloride 1L with potassium chloride over next 4 hours At 12 hours check venous pH, bicarbonate, potassium, capillary ketones made up to 50ml with sodium chloride solution.
4 If MSU Add 10% glucose 125ml/hr if blood glucose falls below 14 mmol/L and glucose patient normally takes long acting insulin analogue Action 5: Establish monitoring regimen Consider reducing the rate of intravenous insulin infusion to Resolution is defined as ketones < mmol/L, venous pH> (glargine, detemir, degludec) continue at usual dose and Hourly capillary blood glucose units/ kg/hour when glucose falls below 14 mmol/L If not resolved review fluid Box 4 Action 1 and insulin infusion Box 3. time Hourly capillary ketone measurement if available More cautious fluid replacement in young people aged 18-25 years, Action 3.
5 Action 3: Assess patient Venous bicarbonate and potassium at 60 elderly, pregnant, heart or renal failure. (Consider HDU and/or central minutes, 2 hours and 2 hourly thereafter If DKA resolved go to Box 6. o Respiratory rate; temperature; blood pressure; pulse; line). oxygen saturation 4 hourly plasma electrolytes Action 3: Assess response to treatment o Glasgow Coma Scale Continuous cardiac monitoring if required Insulin infusion rate may need review if o Full clinical examination Continuous pulse oximetry if required Capillary ketones not falling by at least mmol/L/hr Action 6: Consider and precipitating causes and treat appropria Venous bicarbonate not rising by at least 3 mmol/L/hr BOX 6: Resolution of DKA.
6 Plasma glucose not falling by at least 3 mmol/L/hr Expectation: Patient should be eating and drinking and back on Continue FRIII until ketones less than mmol/L, venous pH > and/or venous bicarbonate over 18 mmol/L normal insulin If ketones and glucose are not falling as expected always check If DKA not resolved identify and treat the reasons for failure to respond. review) the insulin infusion pump is working and connected and that the This situation is unusual and requires senior and specialist input correct insulin residual volume is present (to check for pump Transfer to subcutaneous insulin malfunction).
7 Elderly If equipment working but response to treatment is inadequate, increase Convert to subcutaneous regime when biochemically stable Pregnant (capillary ketones less than mmol/L AND pH over ) and the insulin infusion rate by 1 unit/hr increments hourly until targets achieved. Additional measures patient is ready and able to eat. Do not discontinue intravenous required) Regular observations and Early Warning Score (NEWS2). insulin infusion until 30 minutes after subcutaneous short Accurate fluid balance chart, minimum urine output acting insulin has been given Conversion to subcutaneous Consider urinary catheterisation if incontinent or anuric (not passed urine) insulin should be managed by the Specialist Diabetes Team.
8 If the by 60 minutes team is not available use local guidelines. If the patient is newly Nasogastric tube with airway protection if patient obtunded or persistently diagnosed it is essential they are seen by a member of the specialist vomiting team prior to discharge Measure arterial blood gases and repeat chest radiograph if oxygen Arrange follow up with specialist team saturation less than 92%. BOX 2: Initial fluid replacement Thromboprophylaxis with low molecular weight heparin Consider ECG monitoring if potassium abnormal or concerns about Restoration of circulating volume is priority cardiac status Systolic BP (SBP) below 90mmHg Likely to be due to low circulating volume, but consider other causes such as heart failure, sepsis, etc.
9 BOX 4: 6 to 12 hours Give 500mls sodium chloride solution over 10-15 minutes. If SBP. Aims: Reassess cardiovascular status at 12 hours; further remains <90mmHg repeat whilst awaiting senior input. Most people Ensure clinical and biochemical parameters fluid may be required require between 500-1000mls given rapidly improving Consider involving the ITU / critical care team Continue IV fluid replacement Check for fluid overload Once SBP is >90mmHg, give 1L sodium chloride over the next 60 Avoid hypoglycaemia Assess for complications of treatment fluid minutes. The addition of potassium is likely to be required in this second Action 2 Review biochemical and metabolic overload, cerebral oedema parameters litre of fluid Treat precipitating factors as necessary At 6 hours check venous pH, bicarbonate, Systolic BP on admission 90 mmHg and over Action 1: Re-assess patient, monitor vital signs potassium, capillary ketones and glucose Give 1L sodium chloride over the first 60 minutes If patient not improving by criteria in Box 3, seek Resolution of DKA is defined at ketones < mmol/L.
10 Potassium replacement Potassium replacement mmol/L of senior advice AND venous pH > (do not use bicarbonate as a Represented: Association of British Clinical Diabetologists;. Continue IV fluid via infusion pump at reduced rate British Society for Endocrinology and Diabetes and Potassium level (mmol/L) infusion solution o sodium chloride 1L with KCl over 4 hours marker at this stage). > Nil o sodium chloride with KCl over 6 hours Ensure a referral has been made to the diabetes Association of Children's Diabetes Clinicians; Diabetes team Inpatient Specialist Nurse (DISN) Group; Diabetes UK.