Predetermination request
Found 8 free book(s)Utilization Management Preauthorization Process Overview
www.bcbsil.comPredetermination request via the Availity Attachments tool. Render Care and Services. Check claim status to confirm details. Follow instructions received for next steps. If your request is . approved: If an . adverse determination. is communicated: Submit your claim (Utilization management review is conducted.)
CCD1: Construction Code Determination Form
www1.nyc.govNature of Request . Required for all requests. Only one request may be submitted per form. Determination request is for: Determination Predetermination. Determination request issued to: Borough Commissioner’s Office (Initial) Technical Affairs (Appeal) Elevators: ADMINISTRATIVE USE ONLY. Control #: Appointment date: ...
IMPORTANT: PLEASE READ BEFORE COMPLETING APPLICATION
www.maine.govpredetermination before working as an independent contractor. • If you file this application, it may be: Granted or denied (you will receive a letter to this effect); or, instead of denying it, the Board may return your application and request additional information.
Predetermination Request Form - BCBSOK
www.bcbsok.comA predetermination is a voluntary, written request by a member or a provider to determine if a proposed treatment or service is covered under a patient’s health benefit plan. Predetermination approvals and denials are usually
Dental Benefits – Claim Instructions
www.aetna.com2.PREDETERMINATION OF BENEFITS If total charges for this claim are to exceed the minimum Predetermination dollar amount indicated in the employee's Dental Plan Booklet (and treatment is not emergency in nature), Predetermination of Benefits is suggested. Check the box marked "PRE-TREATMENT ESTIMATE", and complete blocks 30-48.
Alberta Aids to Daily Living Bulletin # 124
open.alberta.caNov 22, 2021 · request through the online health portal. If a suitable wheelchair is not available through the recycle pool, a confirmation will be provided by the recycle vendor. Then the authorizer can submit an authorization request for a new wheelchair along with any applicable supporting documents. Please note that vendors will not be able
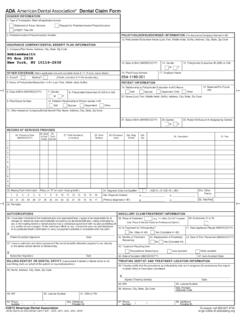
American Dental Association Claim Form
hr.cornell.eduThe form is designed so that the name and address (Item 3) of the third-party payer receiving the claim (insurance company/dental The following information highlights certain …
590154f Dental Claim Form Cigna
www.cigna.comThe form is designed so that the name and address (Item 3) of the third-party payer receiving the claim (insurance company/dental benefit plan) is visible in a standard #9 window envelope (window to the left).