Prescription D Prior Authorization Request Form
Found 9 free book(s)PHARMACY AND THERAPEUTICS COMMITTEE
www.healthpartners.comA. Prior Authorization Request Form B. Hours of Operation ... providing other prescription drug coverage.” New FDA ... HealthPartners Pharmacy Administration to the Part D formulary with a prior authorization status in order to meet CMS requirements, and then receive a
EntyvioConnect Enrollment Form | Entyvio® (vedolizumab)
www.entyviohcp.comPrior Authorization (PA) Support ... can request Nurse Support when they sign up on page 4 FAX completed forms to ... EntyvioConnect Enrollment and Prescription Form FAX page 3 and page 4 to 1-877-488-6814 or call 1-855-ENTYVIO (1-855-368-9846) Monday through Friday, from 8 am to 8 pm ET (except holidays) ...
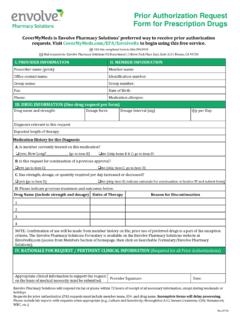
Prior Authorization Request Form for Prescription Drugs
pharmacy.envolvehealth.comPrior Authorization Request Form for Prescription Drugs . CoverMyMeds is Envolve Pharmacy Solutions’ preferred way to receive prior authorization ... Requests for prior authorization (PA) requests must include member name, ID#, and drug name. Incomplete forms will delay processing.
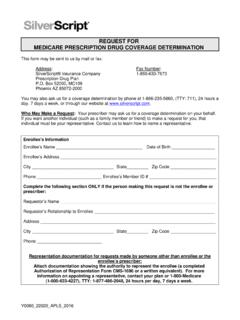
REQUEST FOR MEDICARE PRESCRIPTION DRUG COVERAGE …
www.caremark.comI request prior authorization for the drug my prescriber has prescribed.* I request an exception to the requirement that I try another drug before I get the drug my prescriber prescribed (formulary exception).* I request an exception to the plan’s limit on the number of pills (quantity limit) I …
Programs of All-Inclusive Care for the Elderly (PACE)
www.cms.govThe PACE benefit includes all outpatient prescription drugs, as well as over-the-counter ... and how to access emergency services and that no prior authorization is needed. ... Participants need to understand when to request prior authorization and when to request urgent care. [42 CFR §§ 460.100(e)(2) and (3); 71 FR 71284 and 71297 (Dec. 8 ...
Specialty Substance Use Disorder (SUD) System ...
publichealth.lacounty.govThe Service Request Form is an essential part of utilization management and is the provider’s opportunity to demonstrate a patient is eligible for services (Part A of the Service Request Form) and request preauthorization or authorization for a certain service (Part B of the Service Request Form).
PHARMACY MANUAL POLICY GUIDELINES - eMedNY
www.emedny.orgPrescription Form in order to be dispensed by a pharmacy. Multiple drug orders are not allowed on prescriptions for controlled substances. Refills A prescription or fiscal order may not be refilled unless the prescriber has indicated on the prescription or fiscal order the number of refills and was specifically requested to be
WellCare Value Script (PDP), WellCare Wellness Rx (PDP)
fm.formularynavigator.comchanges based on new clinical guidelines. If we remove drugs from our formulary, or add prior authorization, quantity limits and/or step therapy restrictions on a drug or move a drug to a higher cost-sharing tier, we must notify affected members of the change at l east 30 days before the change becomes effective, or at the time the
Patient Support Program & Patient Assistance Enrollment Form
www.pfizeroncologytogether.comTO BE COMPLETED BY PATIENT 2 OF 7 Be sure your HCP faxes the completed form to 1-877-736-6506 or mail to: Pfizer Oncology Together, PO Box 220366, Charlotte, NC 28222-0366. For questions, please call 1-877-744-5675, Monday–Friday, 8 am–8 pm ET.For details about how we collect and use personal information, including applicable U.S. state
Similar queries
Prior Authorization Request Form, Prescription, HealthPartners, Prior authorization, EntyvioConnect Enrollment Form, Request, Prescription Form, Request prior authorization, Specialty Substance Use Disorder SUD, Request Form, Authorization, EMedNY, WellCare Value Script (PDP), WellCare Wellness Rx, Form