Search results with tag "Prior"
IMPACTS OF PRIOR AUTHORIZATION ON HEALTH CARE …
www.nihcr.org1.2 The Prior Authorization Process 4 1.3 Prior Authorization in Medicare and Medicaid 5 2 EVIDENCE OF IMPACTS ON HEALTH CARE USE AND SPENDING 6 3 EVIDENCE OF BURDENS OF PRIOR AUTHORIZATION 9 3.1 Provider Time and Operating Costs 9 3.2 Delays in Patients Receiving Care 9 3.3 Poorer Health Outcomes 9 4 STRATEGIES TO IMPROVE …
Illinois Uniform Prior Authorization Form
www.bcbsil.comIllinois Uniform Electronic Prior Authorization Form For Prescription Benefits . Important: Please read all instructions below before completing this form. 215 ILCS 5/364.3 requires the use of a uniform electronic prior authorization form when a policy, certificate or contract requires prior authorization for prescription drug benefits.
UnitedHealthcare Medicare Advantage Prior Authorization ...
www.uhcprovider.comFeb 01, 2022 · This prior authorization requirement does not apply to the following plans: Excluded Plans . The UnitedHealthcare Prior Authorization Program does not apply to the following excluded benefit plans. However, these benefit plans may have separate notification or prior authorization requirements. For details, please refer to the
2022 Summary of Changes to WellMed Prior Authorization ...
www.wellmedhealthcare.comFeb 01, 2022 · schedule coverage. For more information about changes in WellMed Prior Authorization program and current prior authorization requirements, please visit WellMed provider portal . ePRG. Texas Florida • WellMed Texas Prior Authorization Requirements will apply in Austin, Corpus Christi, Houston, Dallas & Fort Worth, El Paso, El
Kentucky Medicaid MCO Prior Authorization Request Form ...
www.uhcprovider.comKentucky Medicaid MCO Prior Authorization Request Form . MAP 9 –MCO 2020 MCO Prior Authorization Phone Numbers ANTHEM BLUE CROSS BLUE SHIELD KENTUCKY DEPARTMENT PHONE FAX/OTHER Medical Precertification 1-855-661-2028 1-800-964-3627 www.availity.com ...
Electronic Prior Authorization Flyer - Blue Cross Blue ...
www.bcbsm.comBlue Cross Blue Shield of Michigan and Blue Care Network members. Electronic prior authorization, or ePA, replaces faxing and phone calls so you can focus less on administrative tasks and more on patient care. Electronic prior authorization benefts • Auto approvals for select drugs • Improved turnaround time for review and decisions
CDPHP® Utilization Review Prior Authorization/Medical ...
www.cdphp.com*If DM1: Call provider services to check for coverage; prior authorization is not required for all in network providers. If DM2: Call provider services at (518) 641-3140 to check if prior authorization is required. If required, please fill out and fax this form …
Pharmacy Prior Authorization Request Form
www.mercycareaz.orgFax completed prior authorization request form t800-854-7614 or submit Electronic Prior Authorization through CoverMyMeds® or SureScripts. All requested data must be provided. Incomplete forms or forms without the chart notes will be returned.
Texas - Outpatient Prior Authorization Fax Form
ambetter.superiorhealthplan.comOUTPATIENT Prior Authorization Fax Form Fax to: 855-537-3447. Request for additional units. Existing Authorization. Units (MMDDYYYY) Standard and Urgent Pre-Service Requests - Determination within 3 calendar days (72 hours) of receiving the request * INDICATES REQUIRED FIELD. MEMBER INFORMATION. Date of Birth. Member ID * Last Name, First
TX-PAF-5869 - Medicaid Prior Authorization Fax Form
www.superiorhealthplan.comMEDICAID PRIOR AUTHORIZATION FORM Complete and Fax to: 800-690-7030 Behavioral Health Requests/Medical Records: Fax. 866-570-7517. Transplant: Fax. 833-589-1245 . Request for additional units. Existing Authorization. Units. Urgent requests - I certify this request is urgent and medically necessary to treat an injury, illness or condition (not ...
DURABLE MEDICAL EQUIPMENT (DME) - TMHP
www.tmhp.comOct 10, 2020 · below. Requests for authorization or prior authorization must be submitted in writing. Requests for equipment that requires prior authorization must be completed and received before the requested date of service. The CSHCN Services Program may reimburse providers for both custom and standard (noncustom) DME. 17.2.1 Custom DME
Pharmacy Prior Authorization Form - Anthem
providers.anthem.com3. To help us expedite your authorization requests, please fax all the information required on this form to 1-844-512-7020 for retail pharmacy or 1-844-512-7022 for medical injectables. 4. Allow us at least 24 hours to review this request. If you have questions regarding the prior authorization request, call us at 1-800-901-0020.
Ohio - Outpatient Medicaid Prior Authorization Fax Form
www.buckeyehealthplan.comOUTPATIENT MEDICAID PRIOR AUTHORIZATION FAX FORM Complete and Fax to: SN/ Rehab/LTAC (all requests) 1-866-529-0291 Home Health Care and Hospice (all requests) 1-855-339-5145 DME All DME/Sleep Study/Quantitative Drug Tests/Genetic Testing Requests-1-866-535-4083 PA requests (all other PA requests) 1-866-529-0290 Request for additional units.
Prescription Drug Prior Authorization Form
magellanrx.comPaid under Insurance Name: Prior Auth Number (if known): Other (explain): 2. Administration: Oral/SL Topical Injection IV Other: 3. Administration Location: Physician’s Office Home Care Agency Other (explain): Ambulatory Infusion Center Outpatient Hospital Care Patient’s Home Long Term Care 4.
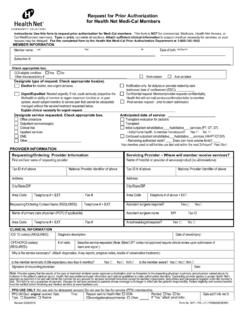
Health Net’s Request for Prior Authorization
www.healthnet.comInstructions: Use this form to request prior authorization for Medi-Cal members. This form is NOT for commercial, Medicare, Health Net Access, or Cal MediConnect members. Type or print; complete all sections. Attach sufficient clinical information to support medical necessity for services, or your request may be delayed.
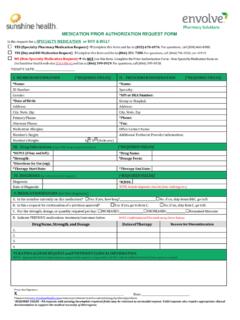
Medication Prior Authorization Request Form - Sunshine …
www.sunshinehealth.comMEDICATION PRIOR AUTHORIZATION REQUEST FORM Is the request for a SPECIALTY MEDICATION or BUY & BILL? YES (Specialty Pharmacy Request) Complete this form and fax to (855) 678-6976. For questions, call (800) 460-8988. YES (Buy and Bill Medication Request) Complete this form and fax to (866) 351-7388. For questions, call (866) 796-0530, ext. 41919.
(required) No - OptumRx
www.optumrx.comPrior Authorization Form General/Non-Preferred Drugs Access this PA form at: ... Buprenorphine Products Celebrex Compounds Daklinza Diabetic Supplies Dipeptidyl-Peptidase IV Inhibitors Growth Hormones Harvoni High Potency Statins Incretin Mimetics Influenza Antivirals I/DD Worksheet Long Acting Narcotics
Form - II FORM FOR GIVING INTIMATION OR SEEKING …
csmrs.gov.inFORM FOR GIVING INTIMATION OR SEEKING PREVIOUS SANCTION UNDER RULE 18(2) OF THE C.C.S (CONDUCT) RULES, 1964 FOR TRANSACTION IN RESPECT OF IMMOVABLE PROPERTY 1. Name and Designation: 2. Scale of pay and present pay: 3. Purpose of application-sanction for transaction/; prior intimation of transaction. 4. Whether property is …
2021 HCPCS Special Bulletin - TMHP
www.tmhp.com• Claims submitted with dates of service on or after January 1, 2021, must be submitted with the new 2021 HCPCS procedure codes, as applicable . The previously-approved authorizations will be automatically updated to the corresponding new procedure codes . Prior Authorization for Discontinued Procedure Codes that Require
Aetna - Medical Exception/Prior Authorization ...
www.aetna.comNew Therapy . Renewal . If Renewal, Date therapy initiated: Route of administration: Oral/SL . Topical . Injection . IV . Other: Administered: Doctor’s Office . Dialysis Center. Home Health . By Patient . Other: Medication Name Dose/Strength . Frequency Length of Therapy Number of Refills Quantity ; List of Previous Drugs Tried Drug Name; Dosage
TATA INSTITUTE OF SOCIAL SCIENCES V.N. Purav Marg, …
www.tiss.edu•Candidates with prior teaching and/or field practice experience of two years will be preferred. •Research and published work in peer-reviewed journals. Other Conditions: •The Institute reserves the right to relax qualifications of the candidate based on the work experience and to relax age in the case of persons already holding comparable positions
2022 CIGNA COMPREHENSIVE DRUG LIST (Formulary)
www.cigna.comApr 01, 2022 · from our drug list, add prior authorization, quantity limits, and/ or step therapy restrictions on a drug or move a drug to a higher cost-sharing tier, we must notify affected customers of the change at least 30 days before the change becomes effective, or at the time the customer requests a refill of the
GUIDANCE NOTE ON APPLICATION FOR PRIOR …
www.justice.gov.za1.5 Any examples provided in this guidance note are not exhaustive and should be regarded as mere guidance. 2 DEFINITION 2.1. “Child” refers to a person under the age of 18 years, as defined in the Children’s Act 38 of 2005; 2.2. “Credit Bureau” refers to a person required to apply for registration as such in
Understanding Formative Assessment - WestEd
www2.wested.orghelp guide instruction. This paper is one in . ... assessment. Subsequent to that, and prior to the conclusion, is a brief review of summaries of research on how formative assess - ment affects student learning. ... students’ learning, or for probing more deeply to gather evidence
Form for Annual Immovable Property Return - DC(MSME
dcmsme.gov.inForm for giving prior intimation or seeking previous sanction under Rule 18(2) of the CSS (Conduct) Rules, 1964 for transaction in respect of immovable Property. 1. Name and Designation : 2. Scale of Pay and Present Pay : 3.Purpose of application sanction :
FORM-I - Comptroller and Auditor General of India
cag.gov.inForm for giving prior intimation or seeking previous sanction under Rule 18 (2) of the CCS (Conduct) Rules, 1964 for transaction in respect of immovable property. (Please read the instructions before filing up the form) 1. Name of the Government servant: (a) Designation: (b) Service to which belongs: (c) Employee No./ Code No.: 2.
How to obtain an Automotive Air Conditioning Licence
www.arctick.orgRecognition of Prior Learning (RPL) and Recognition of Current Competency (RCC) is a process for recognising that you have gained skills, knowledge and experience from other courses, academic education, work experience and training on the job. To use RPL or RCC to obtain the required qualification from a registered training organisation
Fax: Email
alamedaalliance.orgPrior Authorization Request Fax: (855) 891-7174 Phone: (510) 747-4540 Note: All HIGHLIGHTED fields are required. Handwritten or incomplete forms may be delayed. NOTE: The information being transmitted contains information that is confidential, privileged and exempt from disclosure under applicable law.It is intended solely for the use of the ...
LOCKHEED MARTIN CORPORATION CORPDOC 1 GENERAL …
www.lockheedmartin.comCorpDoc 1 (2021) LOCKHEED MARTIN CORPORATION CORPDOC 1 GENERAL PROVISIONS FOR COMMERCIAL SUBCONTRACTS/PURCHASE ORDERS 1. ACCEPTANCE OF CONTRACT/TERMS AND CONDITIONS (a) This Contract integrates, merges, and supersedes any prior offers, negotiations, and agreements concerning the
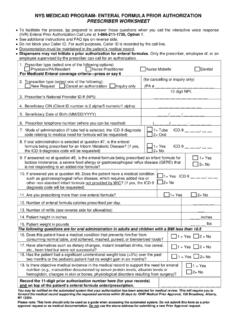
NYS MEDICAID PROGRAM- ENTERAL FORMULA PRIOR …
www.emedny.orgEnteral nutritional formula codes: B4149- B4162 and B9998. Pharmacy Provider manual (Provider Communications section) for the enteral classification list. DME Provider manual (Procedure Codes section) for complete documentation requirements.
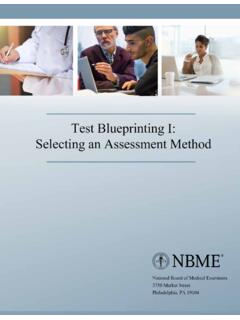
Test Blueprinting I: Selecting an Assessment Method
www.nbme.orgFor each learning objective, indicate the domain in which it is most associated. Learning Objective Cognitive Affective Psychomotor List three causes of aortic stenosis. Offer to and properly drape a female patient prior to auscultation. Correctly identify common systolic murmurs on an audio recording.
EXPERIENCE THE NEW
archives.nseindia.comFeb 08, 2022 · Prior to BSE he was an Executive Director in Morgan Stanley India for 10 years. Earlier at National Stock Exchange where he managed functions like Trading Operations, Inspection, Investigation, Futures & Options Clearing and Trading, CEO of India Index Services and Dotex International 28 years’experience in Capital markets, which includes
Ambetter Outpatient Prior Authorization Fax Form
ambetter.buckeyehealthplan.comoutpatient authorization form. all required fields must be filled in as incomplete forms will be rejected. copies of all supporting clinical information are required. lack of clinical information may result in delayed determination. complete and. fax. to: 888-241-0664. servicing provider / facility information. same as requesting provider
Required Written Notice to Consumers of Their “3-Day Right ...
www.wolfflaw.comRequired Written Notice to Consumers of Their “3-Day Right To Cancel” Certain Residential or Home Improvement Contracts, ... The buyer has a duty to take reasonable care of the goods in his possession both prior to cancellation and during the 20-day period following. During the 20-day period after
RECRUITMENT OF SOCIAL SECURITY OFFICER / MANAGER …
www.esic.nic.infee/ intimation charges (vii) Have a valid personal email ID and mobile no., which should be kept active till the completion of this Recruitment Process. ESIC may send intimation to download call letters for the Examination ... verified to ensure that the same are correct prior to final submission. 4. Candidates are advised to carefully fill ...
Prior Authorization Requirements for UnitedHealthcare
www.uhcprovider.comJan 01, 2022 · Prior authorization required . Prior authorization is required for all states. 29826 29843 29871 Prior authorization is required for all states. In addition, site of service will be reviewed as part of the prior authorization process for the following codes except in AK, MA, PR, TX, UT, VI and WI.
Prior Authorization Request Form - MVP Health Care
www.mvphealthcare.comPrior Authorization Request Form All procedures or health care services requiring prior authorization should be faxed or mailed to the Corporate Utilization Management department at MVP Health Care BEFORE services are scheduled. This completed form and all supporting medical documentation (lab, radiology, consultation reports,
Prior Authorization Form
www.myprime.comThe Illinois Department of Insurance has made a uniform prior authorization (PA) request form available for use by prescribing providers to initiate a prior authorization request. The form should be used when requesting pre-approval from Blue Cross and Blue Shield of Illinois (BCBSIL) for any specified prescription(s) or prescription quantity ...
Prior authorization request form - Aetna
www.aetnabetterhealth.comPhiladelphia, PA 19103 . Prior authorization request form . You must have a valid PROMISe ID (i.e., participate in the Pennsylvania Medicaid programs) at the time the service is rendered in order for your claim to be paid. For more information, please visit https://promise.dpw.state.pa.us .
Prior Authorization and Step Therapy Coverage Criteria ...
www.bcbsm.comThe criteria for medications that need prior authorization or step therapy are based on current medical information and the recommendations of Blue Cross and BCN’s Pharmacy and Therapeutics Committee, a group of physicians, pharmacists and other
Prior Authorization Request Form - American Health Holding
www.americanhealthholding.comPrior treatment provided (i.e., PT, NSAIDS): Related labs/diagnostic studies results (i.e., X-rays, ultrasound labs): Benefits are subject to eligibility and all HealthChoice policy provisions at the time services are incurred.
Similar queries
Prior Authorization, Health, Prior Authorization Form, Form, Medicare Advantage Prior Authorization, Prior authorization requirements, Coverage, Information, Medicaid, Electronic prior authorization, Cross, Blue Cross Blue Shield of Michigan, OUTPATIENT Prior Authorization Fax Form, Authorization, MEDICAID PRIOR AUTHORIZATION, TMHP, Standard, Pharmacy Prior Authorization Form, OUTPATIENT MEDICAID PRIOR AUTHORIZATION FAX FORM, Prior, Outpatient, Health Net, Request for Prior Authorization, Request prior authorization, Request, Pharmacy, OptumRx, Diabetic Supplies, INTIMATION OR SEEKING, INTIMATION OR SEEKING PREVIOUS SANCTION, Sanction, Prior intimation, 2021 HCPCS Special Bulletin, Claims, Authorizations, Aetna, Therapy, Medication, Or step therapy, Guidance note, APPLICATION FOR PRIOR, Guidance, Formative Assessment, Guide, Assessment, Learning, Students, Immovable Property, Prior intimation or seeking previous sanction, Recognition of Prior Learning, 2021, COMMERCIAL, PROGRAM- ENTERAL FORMULA PRIOR, Nutritional formula, Test Blueprinting I: Selecting an Assessment, Outpatient Prior Authorization, Outpatient authorization form, Written Notice, Intimation, Prior authorization request form, Consultation, Prior authorization request, Prior Authorization and Step Therapy, Step therapy