Services that require authorization authorization
Found 6 free book(s)Prior Authorization (General) 1.
www.cms.govneurostimulators. The Final List of Outpatient Services that Require Prior Authorization is located here. 4. Q: What codes require prior authorization for implanted spinal neurostimulators? A: CMS will only require prior authorization for CPT code 63650 (Implantation of spinal neurostimulator electrodes, accessed through the skin) at this time ...
FINAL RULE: CMS-1717-FC: PRIOR AUTHORIZATION …
www.cms.govFINAL RULE: CMS-1717-FC: PRIOR AUTHORIZATION PROCESS and REQUIREMENTS for CERTAIN HOSPITAL OUTPATIENT DEPARTMENT (OPD) SERVICES TABLE 65: FINAL LIST of OUTPATIENT SERVICES THAT REQUIRE PRIOR AUTHORIZATION Federal Register / Vol. 84, No. 218 / Tuesday, November 12, 2019 . Code (i) Blepharoplasty, Eyelid Surgery, Brow Lift, …
Blue Cross and BCN: Procedures that require prior ...
ereferrals.bcbsm.comPrior authorization is required for these cardiac implantable devices and services for dates of service on or after Jan. 1, 2021, for Medicare Plus Blue, BCN commercial and BCN Advantage members. (3) For these procedures, providers must submit the authorization request after, not before, the service has been completed. (4)
Services that require authorization for Michigan providers
ereferrals.bcbsm.comServices that require authorization for Michigan providers For Medicare Plus BlueSM members Updated May 2021 For more complete information about care management and utilization management requirements, refer to the Medicare Plus Blue PPO Provider Manual. 1
Procedures and services requiring prior authorization
modahealth.comPrior authorization is not required but will be reviewed with claim submission for medical necessity. CMS guidelines are applied for prior authorization unless otherwise stated in Moda Health criteria (MHMNC). DME requests $250 or more require prior authorization or may be reviewed for medical necessity upon claim submission.
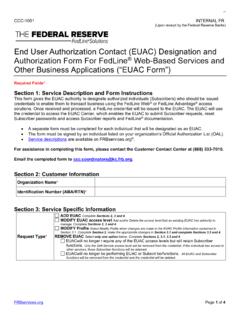
End User Authorization Contact (EUAC) Designation and ...
www.frbservices.orgMar 01, 2019 · End User Authorization Contact (EUAC) Designation and Authorization Form For FedLine ® Web-Based Services a nd ... EUAC longer require any of the EUAC access levels. ... If the individual has access to other services, those Subscriber functions will be retained. EUAC o longer be performing EUAC or Subscriber functions.