Search results with tag "For medicaid"
CARES for Medicaid eligibility, CARES cannot accept this ...
elderaffairs.state.fl.usInstructions for Completing the Medical Certification for Medicaid Long-Term Care Services and Patient Transfer Form AHCA Form 5000-3008, (JUN 2016), incorporated by reference in …
NC Medicaid: State Plan Personal Care Services (PCS), 3L.
files.nc.govMedicaid Beneficiary under 21 Years of Age a. 42 U.S.C. § 1396d(r) [1905(r) of the Social Security Act] Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) is a federal Medicaid requirement that requires the state Medicaid agency to cover services, products, or procedures for Medicaid beneficiary under 21 years of age if the service is
STATE OF MISSOURI MANUAL DISABILITIES WAIVERS …
manuals.momed.com• The person must be eligible for Medicaid in an allowable eligibility category when the services are delivered. • Medicaid does not cover services for individuals residing in a jail or detention facility. • Medicaid waiver services are not available to individuals who are inpatients in a nursing home, ICF/IDD or a hospital.
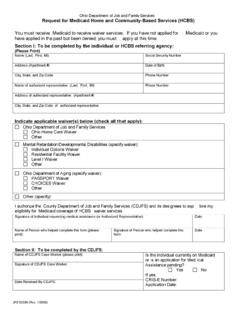
Request for Medicaid Home and Community-Based …
longtermcareohio.comJFS 02399 (Rev. 1/2006) Ohio Department of Job and Family Services Request for Medicaid Home and Community-Based Services (HCBS) You must receive Medicaid to receive waiver services.
Attention DME Providers National Correct Coding …
lamedicaid.comAttention DME Providers . National Correct Coding Initiative (NCCI) Procedure to Procedure Edits . To Be Implemented for DME Providers . The Affordable Care Act requires that States incorporate NCCI edits and methodologies for Medicaid claims
HHSC Medicaid Eligibility -- Reference Guide …
txohc.orgThe Health and Human Services Commission (HHSC) created this guide to provide high-level information to providers regarding eligibility for Medicaid.
GUIDE TO COVERAGE CODES AND HEALTH HOME SERVICES ...
www.health.ny.govJan 01, 2015 · Not covered for Medicaid Services until a spenddown of excess income/resources is met. YES (See notes) Care manager should work with recipients to maintain Medicaid eligibility. 07 EMERGENCY SERVICES ONLY An emergency is defined as a medical condition (including emergency labor and
Medicaid Spenddown - AgeOptions
www.ageoptions.orgMedicaid Spenddown • Helps people who are over income and/or asset eligibility limits qualify for Medicaid • Amount of spenddown depends on a person’s
Similar queries
CARES for Medicaid eligibility, CARES cannot accept, For Medicaid, Medicaid, State Plan Personal Care Services PCS, Eligibility, Department, Services, Attention DME Providers National Correct Coding, Attention DME Providers . National Correct Coding, Providers, HHSC Medicaid Eligibility -- Reference Guide, To maintain Medicaid eligibility, Medicaid Spenddown