Transcription of American Burn Association Practice Guidelines Burn Shock ...
1 SUMMARY ARTICLEA merican burn Association Practice GuidelinesBurn Shock ResuscitationTam N. Pham, MD,* Leopoldo C. Cancio, MD, Nicole S. Gibran, MD*RECOMMENDATIONSS tandardsThere are insufficient data to support a treatmentstandard treatment at this Adults and children with burns greater than 20%TBSA should undergo formal fluid resuscitationusing estimates based on body size and surfacearea burned. Common formulas used to initiate of resuscita-tion estimate a crystalloid need for 2 to 4 ml/kgbody weight/%TBSA during the first 24 hours. Fluid resuscitation, regardless of solution type orestimated need, should be titrated to maintain aurine output of approximately ml/kg/hr in adults and ml/kg/hr in chil-dren. Maintenance fluids should be administered tochildren in addition to their calculated fluid re-quirements caused by injury.
2 Increased volume requirements can be antici-pated in patients with full-thickness injuries, in-halation injury, and a delay in The addition of colloid-containing fluid fol-lowing burn injury, especially after the first 12to 24 hours postburn, may decrease overallfluid requirements. Oral resuscitation should be considered inawake alert patients with moderately sized burnsand is worthy of further study. Hypertonic saline should be reserved to provid-ers experienced in this approach. Plasma sodiumconcentrations should be closely monitored toavoid excessive hypernatremia. Administration of high-dose ascorbic acid maydecrease overall fluid requirements, and is wor-thy of further purpose of this guideline is to review the princi-ples of resuscitation after burn injury, including typeand rate of fluid administration, and the use of ad-junct measures.
3 It presents a rational approach for theinitial treatment of burn guideline is designed to aid those physicians whoare responsible for the triage and initial managementof burn ProblemBurns greater than 20 to 25% TBSA are associatedwith increased capillary permeability and intravascularvolume deficits that are most severe in the first 24hours following injury. Optimal fluid resuscitationaims to support organ perfusion with the leastamount of fluid necessary, at the least physiologicalcost. Under-resuscitation leads to decreased perfu-sion, acute renal failure, and death. Since the adop-tion of weight and injury-size based formulas for re-suscitation, multiple organ dysfunction caused byinadequate resuscitation has become uncommon inmodern American burn care.
4 Instead, administrationof fluid volumes well in excess of 4 ml/kg/% burn hasbeen reported by multiple centers. This phenomenonhas been termed fluid creep. 1 3 Just as under-resuscitation is associated with poor outcome, in-From the *University of Washington burn Center, Seattle,Washington; and Army Institute of Surgical Research,Fort Sam Houston, opinions or assertions contained herein are the private views ofthe authors, and are not to be construed as official or as reflectingthe views of the Department of the Army or Department correspondence to Tam N. Pham, MD, University ofWashington burn Center, Harborview Medical Center, 325 Ninth Ave, Box 359796, Seattle, Washington 2008 by the American burn : fluid administration is associated with adverseoutcomes, such as worsening edema formation, ele-vated compartment pressures, Acute Respiratory Dis-tress Syndrome (ARDS), and multiple organ 6 Hence, what constitutes optimal fluidresuscitation remains a matter of debate.
5 There un-fortunately is a lack of sufficient class I evidence tomake strong recommendations on this clinical prob-lem. However, given the success of various ap-proaches to resuscitate severely burned patients, onemay postulate that the composition of the fluid, theinitial rate of administration and the addition of col-loid are relatively unimportant provided that the cli-nician diligently tailors fluid therapy to the individualpatient and monitors hemodynamic endpoints asso-ciated with adequate tissue Medline search of the English-language literaturewas conducted for the years 1966 to 2007 for allpublications involving the key words burns, ther-mal injury, burn Shock , and resuscitation. Ad-ditional publications were retrieved by searchingthrough references from the available articles.
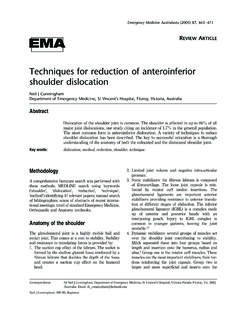
6 Theywere collectively reviewed and summary recommen-dations were made using the following grading scale(Table 1)7: grade A-supported by at least one well-designed prospective trial with clear-cut results, gradeB-supported by several small prospective trials with asimilar conclusion, grade C-supported by a singlesmall prospective trial, retrospective analyses, casesstudies, and expert opinions based on investigators FOUNDATIONBurn Shock PathophysiologySeminal contributions by Baxter and Shires, Artursonand Jonsson, Moyer et al, and others have establishedthat burn Shock begins at the cellular 11 Intheir experimental studies, major burn injuries cause adecrease in cellular transmembrane potential in bothinjured and noninjured tissue. Disruption of thetransmembrane sodium-ATPase activity presumablyaccounts for a rise in intracellular sodium, an effectthat gradually normalizes during the next severaldays.
7 Intracellular sodium shift contributes to hypo-volemia and cellular edema. Heat injury activates therelease of inflammatory and vasoactive mediators re-sponsible for local vasoconstriction and systemic va-sodilation, as well as increased transcapillary perme-ability. Endothelial cells and sensory nerves within theburn wound contribute to the local and systemic in-flammatory response. Released mediators includecomplement proteins, kinins, histamine, serotonin,prostaglandins and oxygen-derived free-radicals, ,13 Disrupted capillary integrity al-lows for rapid equilibration of water, inorganic sol-utes, and plasma proteins (but not cellular elements)between the intravascular and interstitial spaces. Thissequence of events leads to intravascular hypovolemiaand hemoconcentration that are maximal at about 12hours ,15 Thermal injury-induced hypo-volemia consists of a steady loss of intravascular vol-ume that requires sustained replacement to avoidend-organ hypoperfusion and ischemia.
8 In otherwords, the goal of proper fluid resuscitation aims toprevent rather than to treat burn cardiac output is a hallmark of the earlypostinjury phase. Although its precise mechanism re-mains unclear, studies on isolated heart preparationsafter cutaneous burn suggest that impaired intrinsicmyocardial contractility is likely caused by a clinical standpoint, reduced car-diac output is the combined result of decreasedplasma volume, increased afterload, and decreasedcontractility. A recent clinical trial aimed at maximiz-ing preload was able to restore neither preload nornormal cardiac output until 24 hours after , these results mirror earlier observationsmade by Baxter and Shires in their canine model ofburn of scientific evidence*Level of EvidenceRecommendation GradeLevelClass I: large prospectiveclinical trialGrade A:supported by atleastone large prospectiveclinical trial with clear-cutresultsClass II: small prospectiveclinical trial (low power)Grade B: supported by severalsmall prospective clinicaltrials supporting a similarconclusionClass III: retrospectiveanalytical study,contemporaneouscontrolsGrade C: supported by asingle small prospectivetrial, retrospective studiesand consensus expertopinionsClass IV.
9 Retrospectiveanalytical study,historical controlsClass V: case series, expertopinions* Adapted with permission from Sackett DL. Rules of evidence and clinicalrecommendations on the use of antithrombotic agents. Chest 1989;95:2S of burn Care & Research258 Pham, Cancio, and GibranJanuary/February 2008 Optimal Route and Necessity ofFormal ResuscitationThe advent of widely available intravenous cannulashas helped popularize current strategies of intrave-nous resuscitation. An intact gastrointestinal tract cantolerate a large amount of fluid replenishment as ev-idenced by successful oral resuscitation of patientswith infectious diarrheal illnesses throughout ,19In burn patients, oral salt solutions werefrequently used either alone or in combination withintravenous infusion in early studies of burn 22 Although oral resuscitation has been at-tempted for even massive burn injuries, a significantnumber of patients experienced vomiting during thisprocess.
10 This aspect makes enteral resuscitationsomewhat unreliable and impractical, except perhapswhen resources are severely limited. In instanceswhere access to medical care is limited, and providedthat the gastrointestinal tract is uninjured, oral resus-citation can be effectively initiated with balanced saltsolutions. The actual volume each burn patient cantolerate will depend on the magnitude of injury, thepresence of gastric ileus, and the timing of enteraladministration. Early provision of enteral calories mayalso decrease the incidence of adynamic ileus, and isan effective method to supplement volume resuscita-tion. Oral resuscitation is also appropriate for burns 20% since these burns are not associated with severesystemic inflammation, rapid formation of edema,and vasodilation in nonburned ,24 Currentrecommendations are to initiate formal fluid resusci-tation when burns 20% TBSA, preferably throughthe intravenous grade: ResuscitationThere are no available level I or level II publications toguide the choice of isotonic crystalloid 1978 National Institutes of Health workshop onfluid resuscitation did not reach a consensus on thespecific formula nor the type of fluid to be adminis-tered to burn patients.