Transcription of ARTICLES - AC Forum
1 Standardized prophylaxis or treatmentdoses of low-molecular-weight hep-arins (LMWHs) can be used in most pa-tients without dose adjustment. Howev-er, there are concerns about whetherdose adjustments are needed to optimizeanticoagulation in certain patient popula-tions. Specifically, these concerns relateto the potential for increased bleedingdue to LMWH accumulation in patientswith impaired renal function and aboutwhether and when dose adjustments areneeded for obese patients. However, un-warranted down-adjustment of dosingcould compromise clinical article reviews currently avail-able information on the use of LMWHsin patients with impaired renal function orobesity and formulates practical recom-mendations for dosing and monitoring inthese specific subpopulations (Table 1).
2 LMWH Use in Renally ImpairedPatients LMWHs are excreted via the kidney,resulting in a potential for accumulationin patients with impaired renal to pharmacologic and pharmacoki-netic differences, variation may exist inthe rate of accumulation of the differentLMWH compounds in patients with re-nal accumulationmay increase the risk of major bleeding1064nThe Annals of Pharmacotherapy n2009 June, Volume Heparins in Renal Impairment andObesity: Available Evidence and Clinical PracticeRecommendations Across Medical and Surgical SettingsEdith A Nutescu, Sarah A Spinler, Ann Wittkowsky, and William E DagerAnticoagulationAuthor information provided at the end of :To develop practical recommendations for the use of low-molecular-weight heparins (LMWHs) as prophylaxis and treatment of venous thrombo-embolism and acute coronary syndromes in patients with impaired renal functionor obesity.
3 DATASOURCES:Multiple MEDLINE searches were performed (November 2008) toidentify studies for inclusion, using a comprehensive list of search terms including,but not limited to, LMWH, enoxaparin, dalteparin, tinzaparin, obesity, weight, renal,kidney, elderly, monitoring, and anti-Xa. STUDY SELECTION AND DATA EXTRACTION:Only ARTICLES published in English thatwere relevant for this review were SYNTHESIS:In the majority of patients, standardized prophylaxis or treatmentdoses of LMWHs can be used without the need for monitoring and adjustingregimens. For patients with severe renal impairment (estimated creatinine clearance[CrCl] <30 mL/min), doses of some LMWHs should be adjusted or unfractionatedheparin should be used instead. CrCl should be estimated using the Cockcroft-Gaultmethod.
4 Differences are noted in the degree of accumulation of various LMWHs inpatients with moderate-to-severe renal impairment, and thus, the degree of doseadjustment may differ among the various LMWHs. Increasing the prophylacticdoses of LMWH may be appropriate in morbidly obese patients (body mass index 40 kg/m2). The use of total body weight is appropriate for therapeutic doses ofLMWH in obese patients. Laboratory monitoring of the anticoagulation effect ofLMWHs is generally not necessary, but should be considered in patients withmorbid obesity (weight >190 kg), those with severe renal impairment, and thosewith moderate renal impairment with prolonged (>10 days) LMWH use. Whenanti-Xa activity is monitored, it should be determined using a chromogenicmethod and a calibration curve based on the LMWH used.
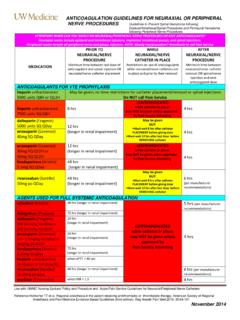
5 CONCLUSIONS:Additional data are needed for specific dose guiding in obese andrenally impaired patients, who are often excluded from larger clinical recommendations are made based on available evidence and authors clinical :anti-Factor Xa activity, chronic kidney disease, dalteparin, dosing,enoxaparin, low-molecular-weight heparin, monitoring, obesity, practice recom-mendations, renal impairment, tinzaparin. AnnPharmacother2009;43 Online, 19 May 2009, , DOI article IS APPROVED FOR CONTINUING EDUCATION CREDITACPEUNIVERSALPROGRAMNUMBER:407-000 -09-008-H01-PARTICLESThe Annals of Pharmacotherapy n2009 June, Volume 43 of LMWH Dosage RecommendationsPatientsRecommendationsDa lteparin PIEnoxaparin PITinzaparin PIRenalCrCl should be estimated in all pts.
6 Anti-Xa may be used to Anti-Xa may be used to impairmentwho are prescribed the anticoagulantmonitor the anticoagulantPts. with renal impairment requireeffect in pts. with severeeffect in pts. with severecareful observation for signs andrenal of with caution in reduction in severe Anti-Xa monitoring can be consideredwith severe renalrenal impairment (CrCl in pts. with severe renal impairment impairment.<30 mL/min) is do not undergo renal Dose adjustment is generally not needed 30 mg once dailynot indicatedprophylaxisin pts. with mild-to-moderate and tinzaparin may not needdose adjustment in pts. with severerenal Use UFH in pts. with severe renal Monitor anti-Xa levels in pts. 1 mg/kg once dailyPts. with severe renal treatmentimpairment (CrCl <20 mL/min).
7 With severe renal impairmentimpairment should beExtended use (>10 days) of LMWHto dose-adjust to anti-Xadosed with caution.(enoxaparin) in pts. with moderatelytarget range of renal function (CrCl 30 60 ) may require anti-Xameasurement and close vigilance torule out drug Use UFH in pts. with severe renal1 mg/kg once dailynot indicatedNSTEMI impairment (CrCl <20 mL/min).Treatment Use UFH in pts. with severe renal not indicatedUse initial 30 mg iv bolus, not indicatedSTEMI impairment (CrCl <20 mL/min).followed by 1 mg/kg reduction is needed in elderly pts.; no initial iv bolus, mg/kg every 12 monitoring and treatment dose adjustments are generally not necessaryfor pts. weighing 190 monitoring can be considered inpts. with morbid obesity (BMI >40 kg/m2).
8 VTEI ncrease prophylaxis doses in pts. withnot indicatedprophylaxismorbid obesity (BMI >40 kg/m2).VTE LMWH dosing should be based on body Use weight-based dosing, withWeight-based dosing is capping at 18,000 for heavy/Dose capping is not dosing may be preferable LMWH dosing should be based on body Use weight-based dosing, with not capping at 10,000 LMWH dosing should be based on body not indicatedUse weight-based dosing,not dose capping of the first 2 doses at 100 of anti-Xa levels is notneeded in clinically stable or uncomp-licated pts. treated with anti-Xa levels should be drawn 4 hafter sc anti-Xa monitoring may be usedto evaluate accumulation at the end ofthe dosing interval in pts. with activity should be determinedusing a chromogenic method and acalibration curve based on the = body mass index; CrCl = creatinine clearance; LMWH = low-molecular-weight heparin; NSTEMI = non ST-segment elevation myocardial infarction;PI = product information; STEMI = ST-segment elevation myocardial infarction; UFH = unfractionated heparin; VTE = venous thromboembolism.
9 ADalteparin indication for long-term treatment of patients with cancer. , patients with severe renal impair-ment treated with LMWHs require careful monitoring forbleeding. It is for this reason that clinical trials of LMWH sgenerally exclude patients with severe renal impairment(Table 2).4-24 Renal function has been classified as: normal glomeru-lar filtration rate (GFR) ( 90mL/min); mildly decreasedGFR (60 89 mL/min); moderately decreased GFR(30 59 mL/min); or severely decreased GFR (15 29mL/min). Patients with a GFR less than 15 mL/min or ondialysis are considered to have end-stage renal disease andare a separate group from patients with severe renal im-pairment (Table 3).25 Creatinine clearance (CrCl) is used asa correlate of GFR and is usually estimated from the Cock-croft-Gault equation, which accounts for serum creatinine(SCr), age, weight, and sex.
10 More recently, the Modifica-tion of Diet in Renal Diseases (MDRD) equation25hasbeen developed to estimate GFR; this equation takes SCr,age, race, and sex into account (Table 3). However, thismethod is not accurate for individuals with an estimatedGFR greater than 60 ,27 SCr alone is not an accu-rate method of predicting renal function,25especially in ,29 Different studies included in this review usedvarious definitions for groups of patients with reduced re-nal function. As a result of differences in methods of esti-mating GFR, variations in the severity scoring of renal fail-ure may arise, resulting in divergent dosing dose adjustments, CrCl should be estimated using theCockcroft- Gault method, in accordance with most controversy in this context is the accuracy ofmeasured anti-Xa activity as a marker for LMWH an-tithrombotic activity or for risk of bleeding.