Transcription of Change Healthcare CLAIMS Provider Information …
1 PAYER ID: SX140 SUBMITTER ID: WEBMDSX131. Change Healthcare CLAIMS Provider Information Form *This form is to ensure accuracy in updating the appropriate account 1 Provider Organization Practice/ Provider Name Facility Name Tax ID Client ID Site ID. Address City STATE ZIP. Contact Name E-mail Address Telephone Fax 2 Vendor ( Change Healthcare certified vendor used to submit files to Change Healthcare ). Vendor Name Vendor Submitter ID. Contact Name E-mail Address 3 Payer Payer ID SX140 partnership health plan OF CA. Group ID Individual Provider ID NPI ID. 4 Confirmations Send Change Healthcare claim Confirmations To: Special Instructions: All Payer Registration forms must contain signatures when applicable, stamped signatures or photo copies are accepted. SUBMIT COMPLETED FORM TO: Fax: (615)231-4843. Email: Testing may or may not be required for this payer, upon approval the payer will communicate to you directly, whether they will require test files from you on your first submissions.
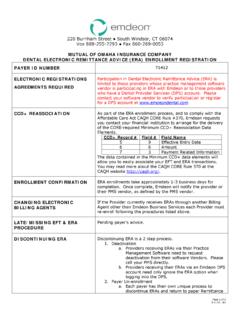
2 In the event you are required to send test files please be sure to send the required files to Change Healthcare as production CLAIMS and contact our CLAIMS support help desk once completed, so that we may be able to communicate to the payer the file name for your submission Change Healthcare REVISION FORM DATE: 06/07/13. Subject: ENROLLMENT - Alert LOB: Institutional/Professional Payer(s): SX140 - CA - partnership healthplan . 12M81 - CA - partnership health plan . Topic: ** IMPORTANT REMINDER **. Be advised that partnership healthplan of California requires an EDI Enrollment Agreement to be completed by any 'NEW' Provider desiring to do EDI CLAIMS business with them. In addition, the payer also requires claim testing before any EDI transactions are accepted into Production. NOTE - If you are already in production and actively doing EDI CLAIMS business with partnership healthplan of CA, and then you may disregard this notice.
3 Action Required by Customer: 1) All 'NEW' Providers desiring to do EDI CLAIMS business with the payer must complete and return to Emdeon for processing an EDI Enrollment Agreement. The EDI Enrollment Agreements can be found here: Institutional - Professional - SUBMIT COMPLETED FORM TO- Fax: (615) 231-4843. Email: 2) Your first claim file of at least 10 CLAIMS per National Provider ID must be submitted in production for testing purposes at partnership healthplan of CA. After submitting these CLAIMS , alert Emdeon of the submission by opening a service request through your normal support process. Emdeon will coordinate the testing with the Payer and notify the Provider when it is complete. This testing process can take approximately 2-3 weeks. Any production claim files received while still in the TEST process, will be rejected by the Payer. To confirm claim production status, please contact CA partnership health plan at (707) 863-4520.
4 Action Taken by Emdeon: Emdeon will receive, process, and transmit (to the Payer) your EDI Enrollment Agreement. The Payer will return the status of the EDI Enrollment Agreement and testing to Emdeon. Thank You for your attention and cooperation, Emdeon partnership healthplan of California 837 CLAIMS Enrollment & Payer Agreement The 837 CLAIMS Enrollment & Payer Agreement Document should be completed and signed by the Trading Partner and the Billing Provider . The Trading Partner is the party that submits electronic CLAIMS directly to partnership healthplan of California (PHC). The Trading Partner and the Billing Provider representatives that sign the 837 CLAIMS Enrollment & Payer Agreement Document indicate that the Trading Partner is authorized to submit claim transactions in HIPAA compliant ANSI X12 formats on behalf of the Billing Provider . Billing Provider should continue to submit paper CLAIMS until they receive notification that the Trading Partner has been approved to submit electronic CLAIMS to PHC on behalf of the Billing Provider listed in the 837 CLAIMS Enrollment & Payer Agreement Document.
5 partnership healthplan of CA accepts electronic files in the HIPAA compliant 5010 version of ANSI X12837 file formats. The completed 837 CLAIMS Enrollment & Payer Agreement Document should be faxed to 707-863-4390 or emailed to: EDI-Enroll After the completed 837 CLAIMS Enrollment & Payer Agreement Document is received, our EDI Team will process it and email the Trading Partner regarding enrollment completion or testing requirements. New Trading Partners will be assigned a submitter ID and will be provided with connection details for EDI file transmissions. To enroll providers for 835 electronic remittance advice files, please complete the form titled 835 ERA Enrollment & Payer Agreement Document.. Trading Partners should not submit electronic CLAIMS on behalf of the billing Provider until they receive confirmation from PHC that enrollment is complete and that the Billing Provider 's NPI number has been set up for electronic CLAIMS submission.
6 partnership healthplan of California 837 CLAIMS Enrollment & Payer Agreement EDI PAYER AGREEMENT. This Electronic Data Interchange (EDI) Payer Service Agreement (the Agreement ) is entered into by and between partnership healthplan of California, a California corporation, with a principal place of business at 4665 Business Center Drive, Fairfield, California 94534 (hereinafter, PHC ), and EMDEON (hereinafter, Trading Partner ). The purpose of this Agreement is to memorialize in writing, the existing connection PHC has with the Trading Partner to submit and receive EDI transactions on behalf of the Provider named in this agreement. In accordance with the health Insurance Portability and Accountability Act (HIPAA) of 1996, PHC must have Business Associate Agreements in place to assure compliance with the rules and regulations dictated by it. TRADING PARTNER'S (SUBMITTER) Information . Trading Partner's Full Legal Name: EMDEON.
7 Trading Partner's Principal Business Address: 3055 LEBANON PIKE SUITE 1000, NASHVILLE, TN 37214. Trading Partner's Mailing Address (if different from principal business address above): Trading Partner's Tax ID #: Trading Partner's State of Incorporation: TN. Trading Partner's Contact Person: Trading Partner's Telephone Number: ENROLLMENT HELP DESK Trading Partner's E-Mail Address: Trading Partner's Fax Number: The Submitter ID is assigned by PHC. Leave blank if Submitter ID has not been assigned by PHC. Submitter ID Number: Approved Trading Partners must submit their Submitter ID in the GS02 element of inbound HIPAA compliant transactions sent to PHC. BILLING Provider 'S Information . Billing Provider 's Name: Billing Provider 's Pay-To NPI Number: Billing Provider 's Contact Person: Billing Provider 's Email Address: Billing Provider 's Telephone Number: Billing Provider 's Fax Number: Billing Provider 's Physical Address: Page 1 of 2.
8 X.