Transcription of COPD 2: management and nursing care - EMAP
1 Copyright EMAP Publishing 2020. This article is not for distribution except for journal club use Clinical Practice Keywords Chronic obstructive pulmonary disease/Respiratory disease Review Respiratory disease This article has been double-blind peer reviewed In this S. afe and effective use of inhaled and oral pharmacological therapies The value of pulmonary rehabilitation Supporting patients to self manage copd 2: management and nursing care Key points Author Stephen Gundry is copd nurse, Newcastle Hospitals NHS Foundation Trust. Nurses have a central role in Abstract Most nurses, not just specialist nurses, will routinely encounter people with the care and chronic obstructive pulmonary disease in their care . Although there is no cure for this management of progressive respiratory disease, nurses have a crucial role in its treatment and people with chronic management , including helping patients to minimise and control their symptoms, and obstructive improve the quality of their lives.
2 This article, the second in a two-part series, pulmonary disease describes treatment and management options when patients are stable and during events, such as exacerbations, when their condition deteriorates. It describes the safe, Inhaled effective use of inhaled and oral drug treatments and oxygen therapy, as well as bronchodilators are non-pharmacological interventions such as smoking cessation, pulmonary the mainstay of rehabilitation support for mental health and helping patients to self manage. drug therapy Citation Gundry S (2019) copd 2: management and nursing care . nursing Times Support for smoking [online]; 116: 5, 48-51. cessation can be M. important in slowing the progression ost nurses not just those opportunity to offer inhaler technique of the disease who are specialist chronic coaching (National Institute for Health and obstructive pulmonary dis- care Excellence, 2018a).
3 If patients have dif- Too few patients ease ( copd ) or respiratory ficulty with an inhaler, they should be are referred for nurses will routinely care for people who offered an alternative. pulmonary have copd . As described in part one of Patients using pressurised metered- rehabilitation this series, copd is a long-term, progres- dose inhalers (pMDI inhalers) should be despite evidence sive respiratory disease, which imposes a given a spacer device; this helps to: of its effectiveness significant health-related burden on the l I ncrease lung deposition of medication;. individual. Although copd cannot be l R educe local oropharyngeal deposition;. Use of self - cured, nurses have a crucial role in the l R educe local side-effects. management plans care and management of people living They should be advised to inhale a single has been shown to with it, including helping them to mini- dose at a time using tidal breathing or a improve patients' mise and control their symptoms, and single breath tidal breathing technique quality of life, while improve the quality of their lives.
4 May be more suitable during episodes of also reducing breathlessness, when it is easier to take sev- breathlessness and Inhaled drug therapies eral (usually five) ordinary-sized breaths hospitalisation Inhaled medication is the mainstay of without the need for a breath hold. It is pharmacological treatment for patients helpful to use combination devices where with copd , inhalers need to be selected on appropriate to minimise the number of the basis of the medication prescribed and inhalers a patient needs (NICE, 2018a). patients' ability to use them with a compe- Medication in dry-powder inhalers tent technique. Most patients can learn to (DPIs) is either built into the device itself or use inhalers effectively with coaching and in capsule form and inserted into the regular review; nurses and other practi- inhaler.
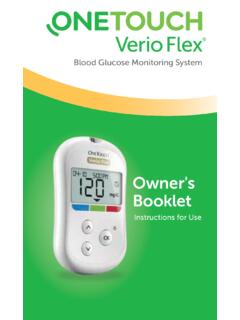
5 DPIs tend to require a greater tioners should use each consultation as an inspiratory effort to inhale the medication nursing Times [online] May 2020 / Vol 116 Issue 5 48 Copyright EMAP Publishing 2020. This article is not for distribution except for journal club use Clinical Practice Review into the airways and should be selected on Fig 1. Inhaled therapies the basis of patients' ability to use them competently. Offer SABA or SAMA to use if needed Short-acting beta-2 agonists (SABAs), such as salbutamol and terbutaline, are used to relieve breathlessness (dyspnoea). and associated exertional limitation. Long- Person still breathless or has exacerbations despite treatments? acting beta-2 agonists (LABAs), such as for- moterol and salmeterol, and long-acting muscarinic antagonists (LAMAs), such as No asthmatic features/features Asthmatic features/features tiotropium, umeclidinium and acli- suggesting steroid responsiveness* suggesting steroid responsiveness*.
6 Dinium, provide ongoing maintenance therapy to help control copd symptoms. They are frequently used in combination. Offer LABA + LAMA Offer LABA + ICS. LAMA/LABA inhalers are suitable for patients who have no asthmatic features in their signs and symptoms. Person still breathless or has Inhaled corticosteroids (ICS) are helpful For ALL inhaled therapies further exacerbations in patients who demonstrate some degree Train people in correct inhaler technique despite further treatment? of steroid responsiveness and asthmatic Review medication, and assess inhaler features, and those who have frequent technique and adherence regularly exacerbations (more than two in a Offer LAMA, LABA and ICS. 12-month period) or hospitalisations. They are generally used in combination inhalers alongside LABA medication, but are asso- Explore further treatment options if needed (see NICE, 2018a).
7 Ciated with increased risk of pneumonia in patients with copd , (Kew and Seniuko- *Any previous secure diagnosis of asthma or atopy, a raised blood eosinophil count, substantial vich, 2014). They should be used with cau- variation in forced expiratory volume per second (FEV1) over time (at least 400ml) or substantial diurnal variation in peak expiratory flow (at least 20%). tion and withdrawn in patients who do not ICS = inhaled corticosteroids; LABA = long-acting beta-2 agonist; LAMA =long-acting muscarinic experience frequent exacerbations. antagonist; SABA = short-acting beta-2 agonist Triple therapy comprising LABA, LAMA and ICS can be considered for patients who remain symptomatic despite NICE (2018b) recommends first-line oral exacerbations per year, prolonged exacer- treatment (NICE, 2018a) (Fig 1).
8 Antibiotic treatment with amoxicillin, dox- bations or exacerbations leading to hos- Patients should be informed about, and ycycline or clarithromycin; options for pital admission (NICE, 2018a). understand: intravenous antibiotics include amoxi- l T he possible side-effects of oral cillin, co-amoxiclav, clarithromycin, co-tri- Oxygen therapy inhalers (for example, oral candidiasis, moxazole and piperacillin with tazobactam. Oxygen therapy is used to correct hypox- hoarse voice, dry mouth); Although routine sputum testing is not aemia, rather than prevent or treat breath- l H ow to reduce their risk of developing recommended, poor response to treatment lessness; it should be prescribed with cau- these side-effects (D'Ancona, 2015); should prompt a change of antibiotic.
9 Tion in patients with copd after arterial l T he role of their inhalers and spacer Oral slow-release theophylline can be blood-gas assessment. An indication to devices; used in patients who are unable to manage refer a patient for long-term oxygen l A ppropriate storage and cleaning inhalers, although there is lower con- therapy assessment is a reliable pulse oxi- instructions. sensus over its efficacy in copd (The Lancet metry reading <92%. Respiratory Medicine, 2018). This requires Long-term oxygen therapy is indicated Oral therapy monitoring plasma levels to titrate the in patients with an arterial partial pressure Oral corticosteroids are not recommended dose correctly, and monitoring patients for of oxygen (PaO2) when stable of < , or for routine maintenance treatment; the medication effects and any adverse <8kPa with comorbid symptoms of periph- patients who cannot be weaned off ster- effects.
10 A reduced dose may be needed for eral oedema, pulmonary hypertension or oids should have their dose reduced to as patients with comorbidities, or when secondary polycythaemia high concen- low as possible and be started on osteopo- starting antibiotics in the macrolide or tration of red blood cells in blood (NICE. rosis prophylaxis, to counter side-effect of fluoroquinolone groups due to possible 2018a). Nurses need to be alert to the safety steroid use (NICE, 2018a). However, oral reduced drug clearance (NICE, 2018a). issues associated with oxygen therapy, corticosteroids have an important role Mucolytic therapy may be helpful in particularly the risk of burns and fire, and during acute exacerbations, patients can patients with a productive cough who falls and trips.