Transcription of Saving Lives, Improving Mothers’ Care
1 Saving Lives, Improving Mothers CareLessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2015-17 Maternal, Newborn and Infant Clinical Outcome Review ProgrammeNovember 2019 Saving Lives, Improving Mothers CareLessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2015-17 November 2019 Marian Knight, Kathryn Bunch, Derek Tuffnell, Judy Shakespeare, Rohit Kotnis, Sara Kenyon, Jennifer J Kurinczuk (Eds.)Maternal, Newborn and Infant Clinical Outcome Review ProgrammeDesign by: Sarah Chamberlain and Andy KirkCover Artist: Tana WestPrinted By: OxuniprintThis report should be cited as:Knight M, Bunch K, Tuffnell D, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ (Eds.)
2 On behalf of MBRRACE-UK. Saving Lives, Improving Mothers Care - Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2015-17. Oxford: National Perinatal Epidemiology Unit, University of Oxford : 978-0-9956854-8-2 Individual chapters from this report should be cited using the format of the following example for chapter 3:Knight M, Clarke B, Head C, James R, Kotnis R, Lucas S, Shakespeare J, Thorne S, Vause S, Youd E and Tuffnell D on behalf of the MBRRACE-UK cardiac chapter-writing group. Lessons on cardiovascular care. In Knight M, Bunch K, Tuffnell D, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ (Eds.)
3 On behalf of MBRRACE-UK. Saving Lives, Improv-ing Mothers Care - Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Mater-nal Deaths and Morbidity 2015-17. Oxford: National Perinatal Epidemiology Unit, University of Oxford 2019: p20-44. 2019 Healthcare Quality Improvement Partnership and National Perinatal Epidemiology Unit, University of OxfordFundingThe Maternal, Newborn and Infant Clinical Outcome Review Programme, delivered by MBRRACE-UK, is commis-sioned by the Healthcare Quality Improvement Partnership (HQIP) as one of the National Clinical Audit and Patient Outcomes Programmes (NCAPOP). HQIP s aim is to promote quality improvement and is led by a consortium of the Academy of Medical Royal Colleges, the Royal College of Nursing, and National Voices.
4 The Clinical Outcome Review Programmes, which encompass confidential enquiries, are designed to help assess the quality of healthcare, and stimulate improvement in safety and effectiveness by systematically enabling clinicians, managers, and policy makers to learn from adverse events and other relevant data. The Maternal, Newborn and Infant Clinical Outcome Review Programme is funded by NHS England, NHS Wales, the Health and Social Care division of the Scottish government, The Northern Ireland Department of Health, and the States of Jersey, Guernsey, and the Isle of Man. MBRRACE-UK - Saving Lives, Improving Mothers Care 2019 ForewordCardiovascular disease remains the leading cause of women s deaths during or after pregnancy in the UK and Ireland.
5 There has been no reduction in the maternal mortality rate from heart disease in the UK for more than 15 years. We must all become more aware that heart disease can and does affect young women, and that the additional strain that pregnancy places on the heart can reveal cardiac complications for the first time. Many of the women whose deaths were reviewed had symptoms which, if they had occurred in a non-pregnant person, would be considered highly suspicious of cardiovascular compromise. Yet they were attributed to normal symptoms of pregnancy. For these women, simply being pregnant led to compromised care and delayed European Society of Cardiology (ESC) guidelines on the management of cardiovascular diseases during preg-nancy were published in 2018, and this report emphasises the importance of a number of the ESC recommendations.
6 In particular, life- Saving treatments such as electrical cardioversion should not be denied to women simply because they are pregnant or postpartum. We should above all aim to ensure that women with known cardiovascular condi-tions enter pregnancy fully informed with their health and medications suitably optimised. The ESC guidelines provide clear direction for pre-pregnancy considerations for women with a wide range of known cardiovascular conditions. In particular, we should continue to be mindful of rare cardiovascular disorders which are very high risk in preg-nancy. Women continue to die from pulmonary hypertension during or shortly after pregnancy, either because their pregnancy is unplanned, or because the diagnosis is never considered in a young woman.
7 Advice on counselling, diagnosis and management is detailed in the ESC there are areas of cardiovascular care emphasised in this report for which we do not yet have clear guidance. Several women died from ischaemic heart disease after becoming pregnant following assisted reproduc-tion. There is no evidence that their cardiovascular health prior to pregnancy was considered, even though they had a number of clear risk factors for heart disease. We urgently need the evidence to guide cardiovascular assessment and screening prior to assisted should be reassured that, although cardiovascular disease is the leading cause of maternal death, the number of women who die during or after pregnancy is still very small.
8 Nevertheless, both women and their health professionals who care for them should be aware of symptoms and signs which are not normal for pregnancy, such as breathlessness when lying flat, chest pain which spreads to the back or arm or fainting during exercise, and which should prompt investigation for cardiovascular disease. By remaining aware of the possibility of heart disease and hence making the diagnosis we will make the first steps to reducing unnecessary deaths amongst young women and leaving families CasadeiVera Regitz-ZagrosekJolien W. Roos-HesselinkPresident of the European Society of Cardiology and British Heart Foundation Professor in Cardiovascular MedicineProfessor of Cardiovascular Disease in Women at the Charit Universit tsmedizin Berlin and Chairperson 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancyProfessor of Cardiology at the Erasmus MC in Rotterdam, The Netherlands and co-Chairperson 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancyMBRRACE-UK - Saving Lives, Improving Mothers Care 2019iKey messagesfrom the report 2019In 2015-17, 209 women died during or up to six weeks after pregnancy.
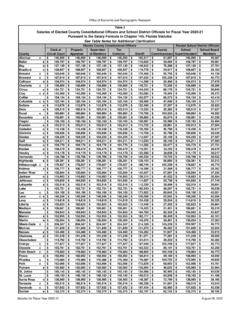
9 From causes associated with their pregnancy, among 2,280,451 women giving birth in the UK. women per 100,000 died during pregnancy or up to six weeks after childbirth or the end of of women s deathsHeart disease can occur for the first time in pregnancy severe chest pain is a red flagWomen who are older, obese, smoke or have diabetes or a family history may be at greater risk of heart diseaseBreathlessness when resting and especially when lying flat is not normal in pregnancy and may indicate heart problemsInequalities in maternal mortalityWomen with risk factors for pre-eclampsia need aspirin to be prescribed from 12 weeks of pregnancyLiving in more deprived areas27%23%19%17%15%37%28%16%10%9%5th quintile (most deprived)
10 4th quintile3rd quintile2nd quintile1st quintile(least deprived)5 per 100,0005 per 100,0007 per 100,00011 per 100,00012 per 100,000 Proportion of women giving birthProportion of women who diedEthnic groupProportion of women giving birthProportion of women who diedWhiteMixedChinese/otherBlackAsianWhi te2%4%4%10%80%4%4%18%16%61%MixedChinese/ otherBlackAsianWhite7 per 100,00013 per 100,00038 per 100,0009 per 100,00023 per 100,000 Age3%15%28%32%4%4%9%26%24%<20 years20 - 2425 - 2930 - 34 4035 - 3911%18%25%13 per 100,0007 per 100,0009 per 100,0006 per 100,00012 per 100,00024 per 100,000 Proportion of women giving birthProportion of women who diedHeart diseaseBlood clotsEpilepsy and strokeOther physical conditionsSepsisMental health conditionsBleedingCancerPre-eclampsiaOth er23%16%13%11%10%10%8%4%2%3%7 women5 women8 women17 women20 women20 women23 women27 women34 women48 womenMBRRACE-UK - Saving Lives, Improving Mothers Care 2019iiExecutive SummaryIntroductionThis report, the sixth MBRRACE-UK annual report of the Confidential Enquiry into Maternal Deaths and Morbidity, includes surveillance data on women who died during or up to one year after pregnancy between 2015 and 2017 in the UK.