Search results with tag "Preauthorization"
Outpatient Preauthorization Caller Guide - BCBSIL
www.bcbsil.comOutpatient Request Preauthorization IVR Caller Guide 2 of 7 Interruption Permitted Preauthorization is required for certain services. A preauthorization determines medical necessity and the appropriateness of treatment. A predetermination may be used to obtain a benefit assessment but is not required. Predeterminations must be submitted in writing.
Provider Preauthorization and Precertification Requirements
www.bcbsm.comPreauthorization is required for outpatient repetitive transcranial magnetic stimulation (rTMS). It may be a benefit for patients with major depressive disorder that meet strict selection criteria. Criteria are available on the Medical policy, precertification and preauthorization router. Coverage is limited to select groups.
Clinical Review Preauthorization Request Form - …
www.connecticare.comCLINICAL REVIEW PREAUTHORIZATION REQUEST FORM - COMMERCIAL Page 1 of 2 08.19.19 . Please use this form for general preauthorization requests and site-of-service reviews. Fax completed form with supporting medical documentation to Clinical Review at 1- 800-923-2882 or 1-860-674-5893.
Blue Cross and Blue Shield of Illinois Provider ... - BCBSIL
www.bcbsil.comrequire benefit preauthorization for certain outpatient services. When you verify eligibility and benefits, you will be able to determine if a group requires benefit preauthorization for outpatient services. Time Frames Benefit preauthorization for elective or non-emergency admissions is required prior to admission or within two
Procedure Code List for Preauthorization for Blue Cross ...
www.bcbsnm.com1 Dec. 6, 2017 . Procedure Code List for Preauthorization for . Blue Cross and Blue Shield of New Mexico . Medicare Advantage Members Only . Beginning Jan.1, 2018, providers will be required to obtain preauthorization through Blue Cross and
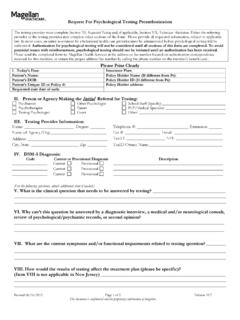
Request for Psychological Testing Preauthorization ...
www.magellanprovider.comRev 12/18 v. 10.8 ©2004-2018 Magellan Health, Inc. Page 1 Request for Psychological Testing Preauthorization Instructions The Request for Psychological Testing Preauthorization form is necessary to authorize psychological testing. This document is designed to …
Blue Cross Community OptionsSM Benefit Preauthorization ...
www.bcbsil.comJune 2017 (Updated December 2017) 1 Blue Cross Community OptionsSM Benefit Preauthorization Requirements (Updated December 2017) This information applies to the following Blue Cross Community Options, or Blue Cross and Blue Shield of
2018 Additional Codes for BCBSTX Preauthorization 2-23-18
www.bcbstx.comFebruary 2018 Procedure Code Description Notes Note: PREAUTHORIZATION
Request for Psychological Testing Preauthorization Form ...
www.magellanprovider.comRequest for Psychological Testing Preauthorization Revised 12/18 Page 1 of 3 Version 10.8 (handwritten submissions) ©2004-2018 Magellan Health, Inc. The testing provider must complete Section XI, Requested Testing and, if applicable, Section XIII, Technician Attestation.Either the
Blue Cross Medicare AdvantageSM Contacts List
www.bcbsnm.com• Preauthorization & Out-of-Network Referrals. 1-877-774-8592 • Preauthorization Fax. 1-855-874-4711 Care Management Programs (Medical & Behavioral Health) 1-855-390-6567 Participating Labs • Quest. 1-800-232-3766 • Lab Corp of America. 1-888-522-2677 The Availity Health Information Network
Summary of Benefits and Coverage: What this Plan Covers ...
www.bcbstx.comPreauthorization may also be required; see your benefit booklet* for details. If you need mental health, behavioral health, or substance abuse services Outpatient services 50% coinsurance for office visits; 30% coinsurance for other outpatient services 50% coinsurance Referral required. Preauthorization may also
Summary of Benefits and Coverage: What this Plan Covers ...
www.bcbstx.comPreauthorization may also be required; see your benefit booklet* for details. If you need mental health, behavioral health, or substance abuse services Outpatient services 40% coinsurance for office visits; 20% coinsurance for other outpatient services Not Covered Referral required. Preauthorization may also
7521 Chiro Guide February 2021 Updated 22521 Master
www.bcbswny.comPreauthorization requirements Preauthorization is required for members with contractual chiropractic visit limitations. Verify eligibility and benefits prior to rendering services by calling Provider Service at 1-800-950-0052 or (716) 882-2616. A Chiropractic Treatment Request (CTR) form is available in the Tools & Resources section of our provider
Summary of Benefits and Coverage Completed Example
www.cms.govPreauthorization is required. If you don't get preauthorization, benefits could be reduced by 50% of the total cost of the service. Physician/surgeon fees . 20% . coinsurance. 40% . coinsurance. 50% . coinsurance. for anesthesia. If you need mental health, behavioral health, or …
2018 BCBSTX Newly Effective Preauthorization …
www.bcbstx.comThis list includes procedure codes related to additional care categories for which benefit preauthorization through Blue Cross and Blue Shield of Texas (BCBSTX) will be required effective Jan. 1, 2018 for the product listed below:
CASHLESS CLAIM FORM Toll Free No. 1800-345 …
www.geninsindia.comCASHLESS CLAIM FORM TO BE FILLED IN BY THE HOSPITAL The issue of this Form is not to be taken as an admission of liability Please include the original preauthorization request from in lieu of PART A
Priority Partners Managed Care Organization …
www.hopkinsmedicine.orgThis section lists the services that do not require a referral or preauthorization • For services provided by participating providers in-office (Place of Service 11), outpatient hospital (Place of Service 22), or ambulatory surgery
Summary of Benefits and Coverage: Coverage …
www.molinahealthcare.com40% : coinsurance after deductible Not Covered . Preauthorization: may be required, or services not covered. Laser corrective eye surgery is not covered.
HealthSelect of Texas Preauthorization Requirements
www.bcbstx.comHealthSelectSM of Texas In-Area (Texas) PRIOR AUTHORIZATION & REFERRAL REQUIREMENTS LIST Effective August 1, 2018 • • • HealthSelect of Texas requires referrals from a PCP using the Blue Essentials℠provider network for network benefits. Prior Authorization …
Summary of Benefits and Coverage: What this Plan ... - UHC
www.uhc.comOutpatient services $25 copay per visit, deductible does not apply 20% coinsurance Network partial hospitalization /intensive outpatient treatment: No Charge Preauthorization required for certain services for out-of-Network or benefit reduces to 50% of allowed. Inpatient services $750 copay per admission, deductible does not apply
BLUE CHOICE PPO FULLY INSURED MEMBERS …
www.bcbstx.comBLUE CHOICE PPOSM FULLY INSURED MEMBERS PREAUTHORIZATION / NOTIFICATION / REFERRAL REQUIREMENTS EFFECTIVE JANUARY 1, 2018 Referrals for Out-of-Network/Out-of-Plan ...
HCAP Highlights - myhcap.com
www.myhcap.comdures that will require preauthorization. Non-expedited preauthori-zation decisions are ren-dered in 1-2 business days from the receipt of
Humana Medicare Advantage Prior Authorization and ...
docs.authorbyhumana.comJan 14, 2022 · *New preauthorization requirement Humana Medicare Advantage Prior Authorization and Notification List (PAL) Effective Date: Jan. 1, 2022 Last Updated: Jan. 14, 2022 . To view the 2022 Medicare Advantage Medication Prior Authorization List, please click . …
Specialty Substance Use Disorder (SUD) System ...
publichealth.lacounty.govThe Service Request Form is an essential part of utilization management and is the provider’s opportunity to demonstrate a patient is eligible for services (Part A of the Service Request Form) and request preauthorization or authorization for a certain service (Part B of the Service Request Form).
FAX COMPLETED FORM WITH SUPPORTING MEDICAL …
www.carefirstchpmd.comPREAUTHORIZATION REQUESTFORM. FAX COMPLETED FORM WITH SUPPORTING MEDICAL DOCUMENTATION TO: 443-552-7407 or 443-552-7408. SECTION 1 - MEMBER INFORMATION ... This request must be accompanied by a physician’s order and/or all other pertinent clinical documentation for appropriate evaluation. Additional documentation may …
Outpatient Services Pre-Authorization Form
irp-cdn.multiscreensite.comOutpatient Services Preauthorization Form Please complete ALL information requested on this form. Incomplete forms will be returned to sender. Please fax this form along with all pertinent patient medical records to: Fax to (859) 253-0099 Attn: Pre-Certification Team If the request is urgent, please call (877) 309-2955 option 2. SUBSCRIBER ...
Summary of Benefits and Coverage: What this Plan Covers ...
www.bcbstx.comIf you have outpatient surgery Facility fee (e.g., ambulatory surgery center) Freestanding Facility: $300/visit plus 20% coinsurance Hospital: $300/visit plus 30% coinsurance Not Covered Referral required. Preauthorization may also be required. For Outpatient Infusion Therapy, see your benefit booklet* for details. Physician/surgeon fees
Fact Sheet 11-01: CHAMPVA Health Care Benefits for the ...
www.va.govpreauthorization is needed • Prescriptions • Doctor’s office visits • Hospital services, in both inpatient and outpatient settings, including emergency room visits • Lab and radiology services • Durable medical equipment. What services are not covered under CHAMPVA? Following is a list of services that are not covered under
Similar queries
Outpatient Preauthorization, BCBSIL, Outpatient, Preauthorization, Clinical Review Preauthorization Request Form -, CLINICAL REVIEW PREAUTHORIZATION REQUEST FORM - COMMERCIAL, FORM, Clinical Review, Blue Shield of Illinois Provider, Procedure Code List for Preauthorization, Mexico . Medicare Advantage Members Only, Request for Psychological Testing Preauthorization, Request for Psychological Testing Preauthorization Instructions, Community OptionsSM Benefit Preauthorization Requirements Updated, Testing, Chiro Guide February 2021 Updated 22521 Master, Request, Summary of Benefits and Coverage, List, Procedure, Preauthorization Requirements, Prior, Referrals, MEMBERS PREAUTHORIZATION / NOTIFICATION / REFERRAL REQUIREMENTS EFFECTIVE, Preauthori-zation, Medicare Advantage Prior Authorization, Medicare Advantage Prior Authorization and Notification List PAL, Effective, Specialty Substance Use Disorder SUD, Request Form, Request preauthorization, Clinical, Pre-Authorization