Search results with tag "Precertification"
A how-to guide for health care professionals who work with us
www.aetna.comPrecertification Code Search tool — allows you to enter up to five CPT codes at a time to quickly determine whether a medical precertification is required for your patient. Online precertification transaction — allows you to add a precertification request for those services that require it and see if a precertification has
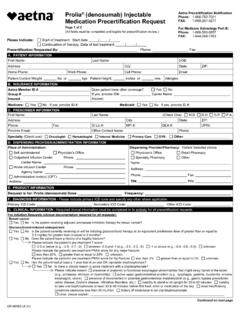
Prolia® (denosumab) Injectable Medication Precertification ...
www.aetna.comProlia® (denosumab) Injectable Medication Precertification Request Aetna Precertification Notification . Phone: 1-866-752-7021 . FAX: 1-888-267-3277 . For Medicare Advantage Part B: Phone: 1-866-503-0857 . FAX: 1-844-268-7263 (All fields must be completed and legible for Precertification Review) Please indicate: Start of treatment: Start date
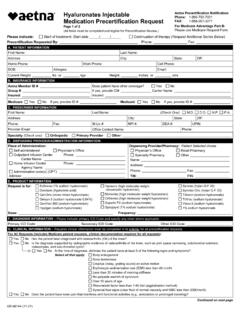
Hyaluronates Injectable Medication Precertification Request
www.aetna.comAetna Precertification Notification Phone: 1-866-752-7021 . Medication Precertification Request. FAX: 1-888-267-3277 . Page 2 of 2 . For Medicare Advantage Part B: (All fields must be completed and legible for Precertification Review.) Please use Medicare Request Form Patient First Name . Patient Last Name . Patient Phone . Patient DOB
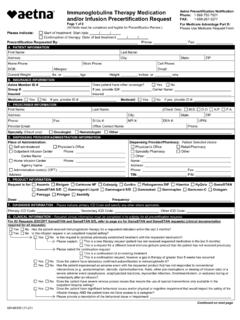
Immune Globulin Therapy Medication Precertification ...
www.aetna.comand/or Infusion Precertification Request Page 2 of 6 (All fields must be completed and legible for Precertification Review.) Aetna Precertification Notification Phone: 1-866-752-7021 FAX: 1-888-267-3277 For Medicare Advantage Part B: Please …
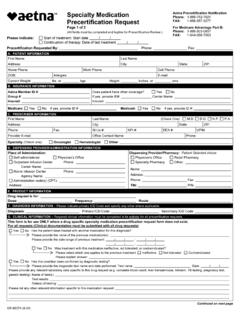
Specialty Medication Precertification Request - Aetna
www.aetna.comAetna Precertification Notification Phone: 1-866-752-7021 FAX: 1-888-267-3277 For Medicare Advantage Part B: Phone: 1-866-503-0857 FAX: 1-844-268-7263 (All fields must be completed and legible for Precertification Review.) Please indicate: Start of treatment: Start date. Continuation of therapy: Date of last treatment. Precertification ...
Pegfilgrastim Precertification Request Aetna ...
www.aetna.comPegfilgrastim Precertification Request (Neulasta ®, Fulphila ®, Nyvepria. TM, Udenyca ®, Ziextenzo ®) Page 2 of 2 (All fields must be completed and legible for precertification review.) Aetna Precertification Notification Phone: 1-866-752-7021. FAX: 1-888-267-3277 . For Medicare Advantage Part B: Please Use Medicare Request Form. Patient ...
Lupron Depot Precert Request - Aetna
www.aetna.comPrecertification Request Aetna Precertification Notification . Phone: 1-866-752-7021. FAX: 1-888-267-3277 . For Medicare Advantage Part B: Phone: 1-866-503-0857. FAX: 1-844-268-7263 (All fields must be completed and legible for Precertification Review) Please indicate: Start of treatment: Start date / / Continuation of therapy, Date of last ...
Services that require precertification* or authorization ...
www.aetna.com**Precertification requirements apply unless state law expressly dictates otherwise. As of January 1, 2019, the following services no longer require precertification or authorization: intensive outpatient, outpatient detoxification (ambulatory withdrawal management) and psychological or neuropsychological testing.
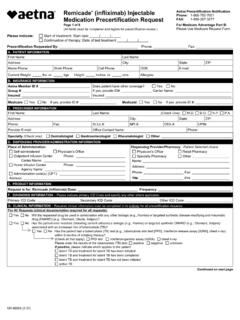
Remicade® (infliximab) Injectable Medication ...
www.aetna.comRemicade® (infliximab) Injectable Medication Precertification Request Aetna Precertification Notification . Phone: 1-866-752-7021 . FAX: 1-888-267-3277 . Page 1 of 8. For Medicare Advantage Part B: (All fields must be completed and legible for precertification review.) Please Use Medicare Request Form . Please indicate: Start of treatment ...
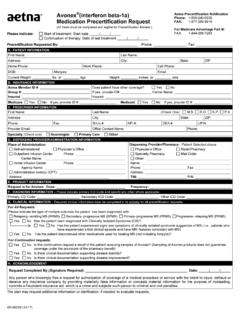
Avonex® (interferon beta-1a) Medication Precertification ...
www.aetna.comAvonex ® (interferon beta-1a) Medication Precertification Request . Aetna Precertification Notification. Phone: 1-855-240-0535 . FAX: 1-877-269-9916
EMPIRE EPO - Welcome to NYC.gov | City of New York
www1.nyc.govYou are responsible for obtaining precertification from Empire’s Medical Management Program for these services provided in-network. For ambulatory surgery, precertification is required for reconstructive surgery, outpatient transplants and opthalmological or eye related procedures. Precertification is also required
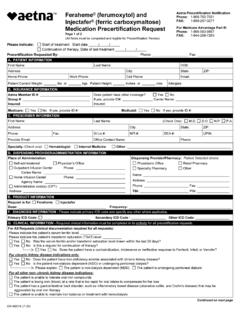
Feraheme® (ferumoxytol) and Injectafer® (ferric ...
www.aetna.com(ferric carboxymaltose) Medication Precertification Request . Aetna Precertification Notification . Phone: 1-866-752-7021 . FAX: 1-888-267-3277 . For Medicare Advantage Part B: Phone: 1-866-503-0857 . FAX: 1-844-268-7263 (All fields must be completed and legible for Precertification Review) Please indicate: Start of treatment: Start date
Botox® (onabotulinumtoxinA) Injectable Medication ...
www.aetna.comMedication Precertification Request . Page 2 of 2 (All fields must be completed and legible for Precertification Review) Aetna Precertification Notification Phone: 1-866-752-7021. FAX: 1-888-267-3277 . For Medicare Advantage Part B: Please Use Medicare Request Form . Patient First Name . Patient Last Name . Patient Phone . Patient DOB . G ...
) Injectable Medication Precertification Request
www.aetna.com(denosumab) Injectable Medication Precertification Request Page 3 of 3 (All fields must be completed and legible for precertification review.) For Medicare Advantage Part B: FAX: 1-844-268-7263 PHONE: 1-866-503-0857 For other lines of business: Please use other form. Note: Xgeva is non-preferred. The preferred product is pamidronate or ...
Services that require precertification - ibxtpa
www.ibxtpa.comServices that require precertification Standard precert list effective: 1/1/2022 This applies to elective, non-emergency services. ... • Cochlear implant surgery • Obesity surgery Reconstructive procedures and potentially cosmetic procedures ... For additional information on the Direct Ship program and the forms needed to request the drugs ...
Procedures, programs and drugs that require …
www.aetna.comOrthognathic surgery Reconstructive as: reconstruction/breast enlargement Shoulder 27. For more information, read all general precertification guidelines • Providers may submit most precertification requests electronically through the secure provider website or using your Electronic Medical Record (EMR) system portal.
Outpatient Behavioral Health (BH) – ABA Treatment Request ...
www.aetna.comRequired Information for Precertification About this form – Do not use for Maryland and Massachusetts You can’t use this form to initiate a precertification or assessment only request. To initiate a request, you have to call the number on the member’s card. Or you can submit your request electronically.
Procedures, programs, and drugs that require precertification
member.aetna.com• For precertification of pharmacy-covered specialty drugs (noted with*) when you are enrolled in a commercial plan, your provider will call 1-855-240-0535. Or, they can fax applicable request forms to 1-877-269-9916. • Your provider can use the drug-specific Specialty Medication Request Form located online under
Provider Preauthorization and Precertification Requirements
www.bcbsm.comPrecertification is not required for: • Outpatient services • Medicare primary contracts • Coordination of benefits contracts All inpatient partial and residential mental health and substance abuse facilities are required to notify New Directions for all admissions and discharges; most admissions will require a clinical review. You may
Procedures, programs and drugs that require precertification
www.aetna.comFor the following services, providers call 1-866-752-7021 for precertification and fax applicable request ... Specialty Medication Request Form located online under ... (daratumumab, J9145) Darzalex Faspro (daratumumab and . care —
Summary of Benefits and Coverage (SBC)
www.ibx.comPrecertification required. Physician/surgeon fees No charge. 20% coinsurance. 30% coinsurance. Not covered. If you need mental health, behavioral health, or substance abuse services Outpatient services$40/Visit. $40/Visit. $40/Visit. Not covered. Precertification required. Inpatient services $350/Day. Max of 5 Copayment(s)/ Admission. $350/Day ...
AT A GLANCE
www.cs.ny.govPrecertification is required unless you are having the test as an inpatient in a hospital. If you do not call, you will pay a larger part of the cost. If the test or procedure is determined not to be medically necessary, you will be responsible for the entire cost.
Aetna Rx - MEDICARE - Botulinum Toxins Injectable ...
www.aetna.comBotulinum Toxins Injectable Medication Precertification Request Page 1 of 3 For Medicare Advantage Part B: FAX: 1-844-268-7263 . PHONE: 1-866-503-0857 . For other lines of business: Please use other form. Note: Botox and Myobloc are non-preferred. The preferred products are Dysport and Xeomin.
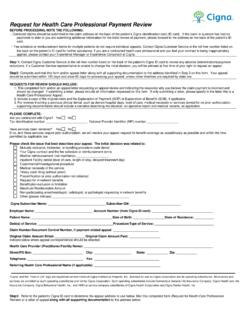
Request for HCP Professional Payment Review
www.cigna.comPrecertification or prior authorization not obtained . Request for in-network benefits . Benefit plan exclusion or limitation . Maximum Reimbursable Amount . Non participating anesthesiologist, radiologist, or pathologist requesting in-network benefits
Blue Cross® and Blue Shield® Service Benefit Plan
www.opm.govHow to request precertification for an admission or get prior approval for Other services 24 Non-urgent care claims 25 Urgent care claims 25 Concurrent care claims 26 . Coverage information 9 . When you lose benefits 11 . General features of our Standard and Basic Options 13 . We have a Preferred Provider Organization \(PPO\) 13
Important Contact Information - Cigna
www.cigna.com• Request precertification for services • Request an exception to the prescription drug list 1.800.88Cigna (882.4462) 1.866.494.2111 Verify the appropriate customer service number on the patient’s ID card Submit or inquire about an Appeal or Dispute 1.800.88Cigna (882.4462) Cigna National Appeals P.O. Box 188011 Chattanooga, TN 37422
Summary of Benefits and Coverage: What this Plan Covers ...
nalchbp.orgYou can call 888-636-6252 to request a copy of either ... Precertification required. $500 penalty for failure to precert. Physician/surgeon fees . 15% coinsurance . 30% coinsurance : Prior authorization is required for spinal and gender reassignment surgery and organ/tissue transplants. If you need mental health, behavioral health, or substance ...
Botox CCRD Prior Authorization Form - Cigna
static.cigna.comIf this is an URGENT request, please call (800) 882-4462 (800.88.CIGNA) ... ** If NEW TO Cigna or precertification is now required, all information must be provided. ... Spinal cord injury Traumatic brain injury Hereditary spastic paraplegia Upper limb spasticity (ULS)
Cervical and Lumbar Spinal Procedures, MPM 25 - phs.org
www.phs.orgprecertification. Musculoskeletal Surgery Services rendered through the Emergency Room are not managed by NIA. All other inpatient and outpatient Musculoskeletal surgery procedures are managed by NIA for the surgeries outlined below. This Medical Policy includes information on the following items (Ctrl+Click to select): Lumbar Spine Surgery
Master Precertification List - Cigna
www.cigna.comFocused ultrasound ablation of uterine leiomyomata, including MR guidance; total leiomyomata volume greater or equal to 200 cc of tissue X X 0075T Transcatheter placement of extracranial vertebral or intrathoracic carotid artery stent(s), including radiologic supervision and
Kentucky Medicaid MCO Prior Authorization Request Form ...
www.uhcprovider.comAetna Better Health of Kentucky UnitedHealthcare Community Plan Humana Healthy Horizons in Kentucky ... Request MUST include medical documentation to be reviewed for medical necessity ... Medical Precertification 1-855-661-2028 1-800-964-3627 www.availity.com
PHYSICIAN REFERRAL FORM - Cigna
www.cigna.comMail: Cigna, Attn: Precertification and Referral Department, 2nd Floor, 1640 Dallas Parkway, Plano, TX 75093 Phone: 866.494.2111 Choose the prompt for “specialist referral.” You will be asked to ... Cigna SureFit, HMO and Network plans require referrals. Please check your patient’s ID card for more guidance.The Cigna C
Summary of Benefits and Coverage: What this Plan Covers ...
www.afspa.orgPrecertification required in U.S. (if not precertified $500 penalty applies). Physician/surgeon fees 10% coinsurance 30% coinsurance Deductible applies for medical services, not surgical services. If you need mental health, behavioral health, or substance abuse services Outpatient services 10% coinsurance 30% coinsurance
Treatment of Gender Dysphoria - Cigna
static.cigna.comUnless otherwise specified in a benefit plan, the following conditions of coverage apply for treatment of gender dysphoria and/or gender reassignment surgery and related procedures, including all applicable benefit limitations, precertification, or other medical necessity criteria.
Your 2022 Prescription Drug List
www.uhc.comPA Prior Authorization (sometimes referred to as precertification)3 — Requires your doctor to provide information about why you are taking a medication to determine how it may be covered by your plan.4 QL Quanty it Limits — Specifies the largest quantity of medication covered per copayment or in a defined period of time.
Preventive Care Services - Cigna
www.cigna.com(MAY require precertification or other reasonable medical management technique or practice depending on benefit plan design) Breast Cancer Screening: women age 40 and older, with or without clinical breast exam, every 1-2 years Note: ACA utilizes the 2002 USPSTF recommendations on breast cancer screening. 77065, 77066
BCBS HIGH DEDUCTIBLE HEALTH PLAN - Blue Cross NC
www.bluecrossnc.com5. Prior Plan Approval (PPA) (precertification before services occur) required for certain health care services. If not precertified, benefits may be denied or paid at 50% of allowed amount. 6. Treatment must meet urgent care criteria. 7. Must meet emergency care criteria. 8.
Your Benefits Choices Guide - My Lowe's Life
www.myloweslife.comIn addition, a plan or issuer may not, under federal law, require that a physician or other healthcare provider obtain authorization for prescribing a length of stay of up to 48 hours (or 96 hours). However, to use certain providers or facilities, or to reduce your out-of-pocket costs, you may be required to obtain precertification. For infor-
Request for Health Care Professional Payment Review - Cigna
www.cigna.comIf no, and these services require prior authorization, we will resolve your appeal request for benefit coverage as expeditiously as possible and within the time ... Precertification or prior authorization not obtained . Request for in-network benefits . Benefit plan exclusion or limitation
Precertification Work Categories
ftp.dot.state.tx.usPrecertification Work Categories . Prime providers and subproviders may be precertified in the technical groups and categories in accordance with the listed requirements. A firm may only use an individual who is employed by that firm at the time of submittal for precertification.
Precertification FAX Request Form - CONFIDENTIAL
medikeeper.blob.core.windows.netPrecertification FAX Request Form - CONFIDENTIAL To submit a Precertification request, please complete the following information and fax all related clinical information to support the medical necessity of this request to AmeriBen Medical Management: URGENT/ STAT REQUEST(s) must be called into Medical Management:
Precertification & Utilization Management - HealthLink
www.healthlink.comadministrator and in accordance with the health benefit program. The list of standard services requiring pre-certification is located online at . https://providerinfosource.healthlink.com > Utilization Management > HealthLink Standard Precertification Listings . For an observation exceeding 23 hours, failure to contact utilization management on the
Precertification request - Amerigroup
provider.amerigroup.comPrecertification request Amerigroup prior authorization: 1-800-454-3730 Fax: 1-800-964-3627 To prevent delay in processing your request, please fill …
Precertification Request - Simply Healthcare Plans
provider.simplyhealthcareplans.comquestion or submit your precertification request, use the following contact information or submit the request online via https://www.availity.com. Statewide Medicaid Managed Care Managed Medical Assistance, Clear Health Alliance and Florida Healthy Kids: Phone: 1-844-405-4296 Fax: 1-800-964-3627
Similar queries
Precertification, Require, Denosumab) Injectable Medication Precertification, Denosumab) Injectable Medication Precertification Request Aetna Precertification, Precertification request, Aetna Precertification Notification, Request, Aetna, Aetna Precertification, Aetna Precertification Notification . Phone, Phone, Require precertification, Infliximab, Injectable Medication, Injectable Medication Precertification Request Aetna Precertification, Interferon beta-1a) Medication Precertification, Interferon beta-1a) Medication Precertification Request, Empire, Ferric, Ferric carboxymaltose) Medication Precertification Request, Injectable Medication Precertification, Surgery, Surgery Reconstructive, Information, Procedures, programs and drugs that require, Breast, Request Form, Medication Request, Daratumumab, Health, Behavioral health, Botulinum, Botulinum Toxins Injectable Medication Precertification Request, Dysport, Professional Payment Review, Important Contact Information, Cigna, List, Spinal, Master Precertification List, Focused ultrasound, Plan, BCBS HIGH DEDUCTIBLE HEALTH PLAN, My Lowe's Life, Categories, HealthLink, Pre-certification