Search results with tag "Medical necessity"
Medicaid Documentation for Medical Professionals
www.cms.govMedical Professionals Medicaid Medical Record Documentation ... To the extent required by the State, Medical necessity and medical rationale are documented and justified in the medical record (remember, each State adopts its own medical necessity definition);[4] ... policy criteria and coding standards as part of the review. 3. Choose a staff ...
Sample Letter of Medical Necessity | HCP.IncyteCARES
hcp.incytecares.comletter of medical necessity will help to explain the physician’s rationale and clinical decision making in choosing a therapy. Please see page 2 for a sample letter of medical necessity with fillable fields that can be customized based on your patient’s medical history and demographic information and then printed.
Clinical Information to Determine Medical Necessity
www.evicore.comlegible medical records pertinent to the test or treatment being requested by the provider. If the medical records provided do not provide sufficiently detailed information to understand the patient’s current clinical status or cannot be read, then medical necessity for the request cannot be established and cannot be approved.
CIGNA STANDARDS AND GUIDELINES/MEDICAL …
www.cigna.comMedical Necessity – In considering coverage for any level of care, all elements of Medical Necessity must be met as specifically outlined in the individual’s benefit plan documents. Although benefit plan definitions of Medical –
Rhythm Management - Boston Scientific
www.bostonscientific.compredicated on Medical Necessity. Note: Medical Necessity is defined by CMS as services or supplies that are: proper and needed for the diagnosis or treatment of the patient ’ s medical condition; are provided for the diagnosis, direct care, and treatment of the patient ’ s medical condition; meet the standards
PREPARING LETTERS OF MEDICAL ... - Prime Engineering
primeengineering.commedical justification, educational needs, and vocational rehabilitation needs. Because we respond to so many questions regarding Medicaid funding of AT, the main topic of this updated and expanded newsletter will be the letter of medical justification or medical necessity, often abbreviated as the LMJ or the LMN. In most cases, what we
Certificate of Medical Neccessity CMS-848-Transcutaneous ...
www.cms.govI have received Sections A, B and C of the Certificate of Medical Necessity (including charges for items ordered). Any statement on my letterhead attached hereto, has been reviewed and signed by me. I . certify that the medical necessity information in Section B is true, accurate and complete, to the best of my knowledge, and I understand
Magellan Healthcare, Inc.* 2021 2022 Magellan Care Guidelines
www.magellanprovider.comMagellan reviews mental health and substance abuse treatment for medical necessity. Magellan defines medical necessity as: “Services by a provider to identify or treat an illness that has been diagnosed or suspected. The services are: 1. consistent with: a. the diagnosis and treatment of a condition; and b. the standards of good medical ...
Save up to 30% on eligible expenses
www.tasconline.com• Wheelchair or autoette (cost of operating/ maintaining) Requiring Additional Documentation The following expenses are eligible only when incurred to treat a diagnosed medical condition. Such expenses require a Letter of Medical Necessity from your physician, containing the medical necessity of the
HRA/FSA Letter of medical necessity - HealthEquity
resources.healthequity.comLetter of medical necessity Under Internal Revenue Service (IRS) rules, some health care services and products are only eligible for reimbursement from your health care FSA, limited purpose FSA, and HRA when your doctor or other licensed health care provider certifies that they are medically necessary.
Checklist: Skilled nursing facility (SNF) documentation
medicare.fcso.comOct 15, 2018 · Also, ensure the medical records provide justification supporting medical necessity for the service by submission of the following documentation: Medical records for 30 days prior to each assessment reference date (ARD) Hospital Documentation . Acute hospital discharge summary and transfer form Medication administration records (MAR)
Speech-Language Pathology Medical Review Guidelines
www.asha.orgMedical Necessity of Speech-Language Pathology Services ..... 8 Why Speech-Language Pathology Services Meet the Definition of Medical ... certification standards while enrolled in a program accredited by the Council on Academic Accreditation in Audiology and Speech-Language Pathology (CAA; ASHA, 2013).
Habilitative Services and Outpatient Rehabilitation Therapy
www.uhcprovider.comCertain state mandates may limit the frequency for requesting plan treatment progress (for example Maryland is limited to no more than one request per year). Related Commercial Policies ... For Medical Necessity Clinical Coverage Criteria For medical necessity clinical coverage criteria, refer to the InterQual ...
2020-2021 NIA Clinical Guidelines for Medical Necessity …
www1.radmd.comGuidelines for Clinical Review Determination Preamble Magellan is committed to the philosophy of supporting safe and effective treatment for patients. The medical necessity criteria that follow are guidelines for the provision of diagnostic imaging. These criteria are designed to guide both providers and reviewers to the most
State of Maryland Medical Necessity Criteria
maryland.optum.comMedical necessity for admission to an RTC level of care must be documented by the presence of all the criteria given below in Severity of Need and Intensity of Service. The child or adolescent must have a mental health disorder amenable to active clinical treatment.
Ambetter Provider Claims & Payments FAQ
ambetter-es.coordinatedcarehealth.com*Ensure the denial letter is included the corrected claim. If a paper claim is filed it must be sent on ... requires a review of the claim with medical records to verify medical necessity to prevent incorrect billing. ... Email an image of the check to your Provider Network Specialist for …
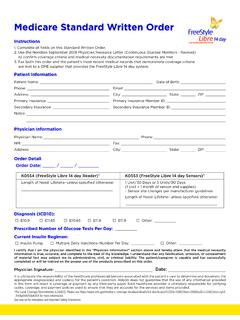
Medicare Standard Written Order - MyFreeStyle
provider.myfreestyle.com2. Use the Noridian September 2018 Physician Resource Letter (Continuous Glucose Monitors - Revised) to confi rm coverage criteria and medical necessity documentation requirements are met. 3. Fax both this order and the patient’s most recent medical records that demonstrate coverage criteria
Improving Your Documentation: Now More Than Ever, Your ...
www.lota.orgpractices, nursing homes, home health agencies, durable medical equipment suppliers and any other provider or supplier that bills Medicare Parts A and B. ... Medical Necessity ... Evaluation/Assessment Evaluation/Assessment Should be: • Concise • Complete • Objective
Medicaid Coverage of Non-Emergency Medical …
www.macpac.govStates may limit the benefit based on medical necessity or utilization control (42 CFR 440.230(d)). For example, some states require prior authorization from the state for trips or place limits on the number of trips Medicaid will cover. For example, Indiana limits the benefit to 20 trips per 12 months (FSSA 2019). Others charge co-payments.
DEPARTMENT OF HEALTH & HUMAN SERVICES
www.medicaid.govAug 30, 2021 · Finally, states may apply medical necessity criteria and other amount, duration, and scope parameters to COVID-19 testing covered under section 1905(a)(4)(F) of the Act and the other amendments made by section 9811 of the …
CMS Manual System
www.cms.govNumber Requirement Responsibility A/B MAC DME MAC Shared-System Maintainers Other A B HHH FISS MCS VMS CWF 9189.1 For all medical necessity reviews,
For Non-Emergency Transports Only ... - Superior Ambulance
www.superiorambulance.comand Family Services and other payers to support the determination of medical necessity for Medicar/Service Car services. I also certify that I am a representative of the facility initiating this order and that our institution has furnished care or other …
ICD-10: Clinical Concepts for Internal Medicine
www.cms.govQuality clinical documentation is essential for communicating the intent of an encounter, confirming medical necessity, and providing detail to support ICD-10 code selection. In support of this objective, we have provided outpatient focused . scenarios to illustrate specific ICD-10 documentation and coding nuances related to your specialty.
cpt codes for Applied behavior Analysis
www.abainternational.orgKnow payor policies and requirements for medical necessity and coverage of ABA services, as well as the terms for modification of agreements. • Compliance with contract provisions and payor requirements regarding claims documentation is essential, especially in light of recent billing fraud cases and heightened scrutiny of billing for ABA ...
Repetitive, Scheduled Non-Emergent Ambulance Transport ...
www.cms.govDec 01, 2015 · The medical necessity requirements for Medicare coverage of ambulance services are set forth in 42 CFR §410.40(e). Medicare covers ambulance services including air ambulance (fixed wing ... Medicare coverage of ambulance services can be found in 42 CFR §§410.40, 410.41, and in the publication 100-02 Medicare Benefit Policy Manual, Chapter 10.
Transportation Services – Medicare Advantage Policy …
www.uhcprovider.comdetermining factor in whether medical necessity is met. Guidelines Emergency Ambulance Services (Ground) Emergency response means responding immediately at the BLS or ALS1 level of service to a 911 call or the equivalent in areas without a 911 call system. An immediate response is one in which the ambulance provider or supplier begins as ...
SMD # 21-005 RE: UPDATED: Mandatory Medicaid Coverage …
www.medicaid.govApr 13, 2022 · medical necessity criteria, provider qualifications and limits on the amount, duration, and scope ... Director Letter is the only guidance we have issued addressing Medicaid coverage of routine ... streamlined uniform form developed for state use by the Secretary, which is currently under
Molecular Diagnostic Infectious Disease Testing
www.uhcprovider.comWhen the documentation does not meet the criteria for the service rendered or the documentation does not establish the medical necessity for the services, such services will be denied as not reasonable and necessary under Section 1862(a)(1)(A) of the Social Security Act.
POWER WHEELCHAIR EVALUATION AND DOCUMENTATION
www.miota.orgParticipants will be able to discuss the Detailed Product Description/Letter of Medical Necessity Participants will be able to discuss the components of the Medicare Power Wheelchair ... Denial will occur if you state the home is not wheelchair accessible and there are no plans for home modification. SPECIALITY THERAPIST EVALUATION ...
Request for HCP Professional Payment Review
www.cigna.comMedical necessity of the service . Timely claim filing (without proof) Precertification or prior authorization not obtained . Request for in-network benefits . Benefit plan exclusion or limitation . Maximum Reimbursable Amount . Non participating anesthesiologist, radiologist, or pathologist requesting in-network benefits
Provider Appeal Form - bcidaho.com
providers.bcidaho.comPlease include the email contact number assigned in your initial inquiry response. Contact #: Please also include your Prior Authorization Reference number if applicable. Reference #: This form should only be used for reasons documented in your provider contract, such as: • Medical Necessity • Investigational • Clinical Editing
Skilled Nursing Facility Consolidated Billing as It ...
www.cms.govA trip to the beneficiary’s home to receive services from a Medicare-participating home health ... transportation to a physician's office and meets the general medical necessity requirement for ... other than an ambulance (for example, via wheelchair van), the wheelchair van would not be …
Clinical Appropriateness Guidelines: Advanced Imaging
aimspecialtyhealth.com“Guidelines”) are designed to assist providers in making the most appropriate treatment decision for a specific clinical condition for an individual. As used by AIM, the Guidelines establish objective and evidence-based, where possible, criteria for medical necessity determinations. In the process, multiple functions are accomplished:
Genetic Testing for Hereditary Cancer Susceptibility Syndromes
static.cigna.comguidelines. In certain markets, delegated vendor guidelines may be used to support medical necessity and other coverage determinations.. Overview . This Coverage Policy addresses genetic testing for germline pathogenic or likely pathogenic variants related to hereditary cancer susceptibility syndromes.
CLINICAL APPROPRIATENESS GUIDELINES
aimspecialtyhealth.com“Guidelines”) are designed to assist providers in making the most appropriate treatment decision for a specific clinical condition for an individual. As used by AIM, the Guidelines establish objective and evidence-based criteria for medical necessity determinations where possible. In the process, multiple functions are accomplished:
Procedure Code Modifiers
provider.indianamedicaid.comJan 01, 2022 · or national coding updates, inclusion of a code on the code tables does not ... and is separately reimbursable based on medical necessity ... EC Informational Erythropoiesis stimulating agent (ESA) administered to treat anemia not due
Inpatient Psychiatric Hospitalization- Supplemental Coding ...
downloads.cms.govServices not meeting medical necessity guidelines should be billed with modifier -GA or -GZ. Refer to CMS Publication 100-04, Medicare Claims Processing Manual, Chapter 30, revised 09/05/2008, for complete instructions.
Medical Necessity Criteria - Blue Cross Blue Shield of ...
www.bcbsm.comMedical Necessity Please refer to the controlling specific health plan and/or group documents for the definition of Medical Necessity. An internal New Directions committee of behavioral health practitioners and psychiatrists developed the Medical Necessity Criteria (“Criteria” or “MNC”) contained in this document. A panel of external,
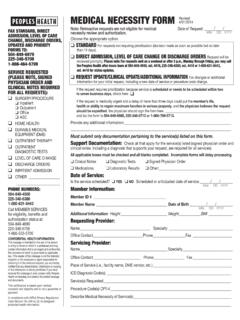
Medical Necessity Form Rev 8.16 - Peoples Health
www.peopleshealth.comnecessity review must still meet InterQual criteria, Medicare guidelines and/or Peoples Health policy, and are subject to retrospective review. *If your contract with Peoples Health specifies that different or additional services than those listed on this form require medical necessity review,
Medical Services Plan - British Columbia
www2.gov.bc.caambulance service obtained outside British Columbia. ... If you are leaving Canada to obtain medical services, the B.C. specialist must write to HIBC (see General Contact Information section) and provide information regarding the medical necessity for a referral outside of Canada. Non-emergency services that are undertaken without prior
Medical Necessity & Charting Guidelines
www.utcomchatt.org5 InterQual Guidelines for InterQual Guidelines for Medical Necessity Utilized for Medicare patient Acute Care inpatient or Observation – – Severity of Illness (SI)
Medical Necessity Form - ASIFlex
webdocs.asiflex.comFSA Letter of Medical Necessity Under Internal Revenue Service (IRS) rules, some health care services and products are only eligible for reimbursement from your Health Care Flexible Spending Account (HCFSA) when your doctor or other
Medical Necessity Letters - Washington Autism Alliance
washingtonautismalliance.orgLetter #2: Intense Behavioral Interventions These recommendations are usually for a large number of therapy hours per week and supervision of the therapists. Even if covered, the number of hours are usually subject to limitations. Tips for Writing Letters for Insurance Coverage of Recommended Therapies PAGE 1 OF 3
Similar queries
Medicaid Documentation for Medical Professionals, Medical, Medical Necessity, Standards, CIGNA STANDARDS AND GUIDELINES/MEDICAL, Rhythm Management, Boston Scientific, OF MEDICAL, Medical justification, Letter of medical justification, Certificate of Medical, Certificate of Medical Necessity, Wheelchair, Form, State, Maryland, Criteria, Guidelines, Medical necessity criteria, State of Maryland Medical Necessity Criteria, Letter, Email, Documentation: Now More Than Ever, Home, Evaluation, Of Non-Emergency Medical, Documentation, Codes for Applied behavior Analysis, Repetitive, Scheduled Non-Emergent Ambulance Transport, Of ambulance services, Ambulance Services, Ambulance, Services, Medicare Advantage Policy, Molecular Diagnostic Infectious Disease Testing, Professional Payment Review, Skilled Nursing Facility Consolidated Billing as, Procedure Code Modifiers, Coding, Erythropoiesis stimulating, Necessity, Medical services, Charting Guidelines, Acute, FSA Letter of Medical Necessity, Flexible Spending Account