Transcription of 5.1. GENERAL TEXTS ON MICROBIOLOGY - …
1 EUROPEAN PHARMACOPOEIA Methods of preparation of sterile GENERAL TEXTS ONMICROBIOLOGY01/2008 METHODS OF PREPARATIONOF STERILE PRODUCTSS terility is the absence of viable micro-organisms. Thesterility of a product cannot be guaranteed by testing; ithas to be assured by the application of a suitably validatedproduction process. It is essential that the effect of thechosen sterilisation procedure on the product (includingits final container or package) is investigated to ensureeffectiveness and the integrity of the product and that theprocedure is validated before being applied in practice. It isrecommended that the choice of the container is such asto allow the optimum sterilisation to be applied. Failure tofollow meticulously a validated process involves the risk of anon-sterile product or of a deteriorated product. Revalidationis carried out whenever major changes in the sterilisationprocedure, including changes in the load, take place.
2 It isexpected that the principles of good manufacturing practice(as described in, for example, the European CommunityGuide to GMP) will have been observed in the design of theprocess including, in particular, the use of: qualified personnel with appropriate training, adequate premises, suitable production equipment, designed for easy cleaningand sterilisation, adequate precautions to minimise the bioburden priorto sterilisation, validated procedures for all critical production steps, environmental monitoring and in-process precautions necessary to minimise the pre-sterilisationbioburden include the use of components with an acceptablelow degree of microbial contamination. Microbiologicalmonitoring and setting of suitable action limits may beadvisable for ingredients which are liable to be contaminatedbecause of their origin, nature or method of methods described here apply mainly to theinactivation or removal of bacteria, yeasts and biological products of animal or human origin or incases where such material has been used in the productionprocess, it is necessary during validation to demonstratethat the process is capable of the removal or inactivationof relevant viral contamination.
3 Guidance on this aspectis provided in, for example, the appropriate EuropeanCommunity Notes for possible, a process in which the product issterilised in its final container (terminal sterilisation) ischosen. When a fully validated terminal sterilisation methodby steam, dry heat or ionising radiation is used, parametricrelease, that is the release of a batch of sterilised items basedon process data rather than on the basis of submitting asample of the items to sterilitytesting,maybecarriedout,subject to the approval of the competent terminal sterilisation is notpossible, filtration througha bacteria-retentative filter or aseptic processing is used;wherever possible, appropriate additional treatment ofthe product (for example, heating of the product) in itsfinal container is applied. In all cases, the container andclosure are required to maintain the sterility of the productthroughout its Assurance Level (SAL)Where appropriate reference is made within the methodsdescribed below, to a sterility assurance level or SAL.
4 The achievement of sterility within any one item in apopulation of items submitted to a sterilisation processcannot be guaranteed nor can it be demonstrated. Theinactivation of micro-organisms by physical or chemicalmeans follows an exponential law; thus there is alwaysa finite statistical probability that a micro-organism maysurvive the sterilising process. For a given process, theprobability of survival is determined by the number, typesand resistance of the micro-organisms present and by theenvironment in which the organisms exist during SAL of a sterilising process is the degree of assurancewith which the process in question renders a population ofitems sterile. The SAL for a given process is expressed as theprobability of a non-sterile item in that population. An SALof 10 6, for example, denotes a probability of not more thanone viable micro-organism in 1 106sterilised items of thefinal product.
5 The SAL of a process for a given product isestablished by appropriate validation AND CONDITIONS OF STERILISATIONS terilisation may be carried out by one of the methodsdescribed below. Modifications to, or combinations of, thesemethods may be used provided that the chosen procedureis validated both with respect to its effectiveness and theintegrity of the product including its container or all methods of sterilisation the critical conditions ofthe operation are monitored in order to confirm that thepreviously determined required conditions are achievedthroughout the batch during the whole sterilisation processThis applies in all cases including those where the referenceconditions are STERILISATIONFor terminal sterilisation it is essential to take into accountthe non-uniformity of the physical and, where relevant,chemical conditions within the sterilising chamber.
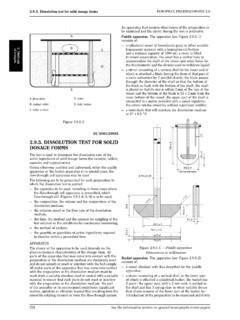
6 Thelocation within the sterilising chamber that is least accessibleto the sterilising agent is determined for each loadingconfiguration of each type and size of container or package(for example, the coolest location in an autoclave). Theminimum lethality delivered by the sterilising cycle and thereproducibility of the cycle are also determined in order toensure that all loads will consistently receive the established a terminal sterilisation process,knowledgeofitsperformanceinrouti neuseisgainedwherever possible, by monitoring and suitably recording thephysical and, where relevant, chemical conditions achievedwithin the load in the chamber throughout each sterilisation (Heating in an autoclave).Sterilisationby saturated steam under pressure is preferred, whereverapplicable, especially for aqueous preparations. For thismethod of terminal sterilisation the reference conditions foraqueouspreparationsareheatingataminim umof121 Cfor 15 min.
7 Other combinations of time and temperaturemay be used provided that it has been satisfactorilydemonstrated that the process chosen delivers an adequateand reproducible level of lethality when operating routinelywithin the established tolerances. The procedures andGeneralNotices(1) Methods of preparation of sterile productsEUROPEAN PHARMACOPOEIA ,astogiveanSALof10 6orbetter. Guidance concerning validation by means of the F0concept is provided below ( ).Knowledge of the physical conditions (temperatureand pressure) within the autoclave chamber during thesterilisation procedure is obtained. The temperature isusually measured by means of temperature-sensing elementsinserted into representative containers together withadditional elements at the previously established coolest partof the loaded chamber. The conditions throughout each cycleare suitably recorded, for example, as a temperature-timechart, or by any other suitable a biological assessment is carried out, this is obtainedusing a suitable biological indicator ( ).
8 Dry heat sterilisation. For this method of terminalsterilisation the reference conditions are a minimumof 160 C for at least 2 h. Other combinations of timeand temperature may be used provided that it has beensatisfactorily demonstrated that the process chosen deliversan adequate and reproducible level of lethality whenoperated routinely within the established tolerances. Theprocedures and precautions employed are such as to give anSAL of 10 6or heat sterilisation is carried out in an oven equipped withforced air circulation or other equipment specially designedfor the purpose. The steriliser is loaded in such a way of the temperature within the steriliser duringthe sterilisation procedure is usually obtained by means oftemperature-sensing elements inserted into representativecontainers together with additional elements at thepreviously established coolest part of the loaded temperature throughout each cycle is suitably a biological assessment is carried out, this is obtainedusing a suitable biological indicator ( ).
9 Dry heat at temperatures greater than 220 C is frequentlyused for sterilisation and depyrogenation of glassware. Inthis case demonstration of a 3-log reduction in heat resistantendotoxin can be used as a replacement for biologicalindicators ( ).Ionising radiation sterilisation. Sterilisation by this methodis achieved by exposure of the product to ionising radiationin the form of gamma radiation from a suitable radioisotopicsource (such as cobalt 60) or of a beam of electrons energisedby a suitable electron some countries there are regulations that lay down rulesfor the use of ionising radiation for sterilisation purposes,for example, in the appropriate European CommunityNotes for this method of terminal sterilisation the referenceabsorbed dose is 25 kGy. Other doses may be used providedthat it has satisfactorily been demonstrated that the dosechosen delivers an adequate and reproducible level oflethality when the process is operated routinely within theestablished tolerances.
10 The procedures and precautionsemployed are such as to give an SAL of 10 6or the sterilisation procedure the radiation absorbed bythe product is monitored regularly by means of establisheddosimetry procedures that are independent of dose are calibrated against a standard source at areference radiation plant on receipt from the supplier and atsuitable intervals of not longer than one year a biological assessment is carried out, this is obtainedusing a suitable biological indicator ( ).Gas sterilisation. This method of sterilisation is only to beused where there is no suitable alternative. It is essentialthat penetration by gas and moisture into the material tobe sterilised is ensured and that it is followed by a processof elimination of the gas under conditions that have beenpreviously established to ensure that any residue of gas orits transformation products in the sterilised product is belowthe concentration that could give rise to toxic effects duringuse of the product.