Transcription of Advanced Hemodynamic Monitoring Swan-Ganz Pulmonary …
1 Advanced Hemodynamic Monitoring Swan-Ganz Pulmonary Artery Catheter The Advanced technology Swan-Ganz catheter, using the same functionality as the standard Swan-Ganz catheter, provides the ability to continuously monitor the balance between oxygen delivery and consumption and investigate the root cause of an imbalance through analysis of the components of stroke volume (preload, afterload, and contractility). Advantages of Continuous Cardiac Output (CCO) Oxygen delivery and consumption Reflection spectrophotometry Swan-Ganz catheter as compared to the Intermittent Determinants of the Swan-Ganz catheter HemoSphere Advanced Monitoring system continuous mixed venous oxygen saturation Monitoring Cardiac Output (iCO) Swan-Ganz catheter Output: SvO2. Additional Advanced diagnostic information with same procedure 60-80% mixed venous Continuous Monitoring of CO, SvO2, EDV and RVEF oxygen saturaton (SvO2). Increased accuracy of cardiac output calculations, elimination of ventilator cycle and thermal noise effect Fiberoptic Mitigation of: transmission User error in association with wedge procedure/calculation Receiving through automated alternative preload parameter (RVEDV) fiber CCO Hemoglobin Oxygenation Metabolic Inappropriate preload assessment secondary to changes 4 8 lpm Hgb 12 16 g/dL SaO2 98% demand VO2.
2 In ventricular compliance affecting PAD or PAOP Hct 35 45% PaO2 >80 200 250. mmHg mL/min P. ulmonary artery rupture potential associated with wedge procedure by providing automated preload parameter (RVEDV). Inappropriate therapy due to miscalculation of PAOP by using Bleeding SaO2 Shivering automated preload parameter (RVEDV) Sending Iatrogenic infection risk from bolus injections fiber Cardiac output error with CCO automation through elimination Photodetector of bolus cardiac output user error Optical module Flowing blood HR SV Hemodilution PaO2 Fever 60 80 bpm 60 100. mL/beat CCO catheter Catheter Pulmonary Thermodilution continuous cardiac output catheter artery Continuous cardiac output measurement is made by periodically warming the blood in the right Optimal HR Anemia FiO2 Anxiety atrium or ventricle with a known quantity of heat. The catheter thermistor detects the small change LEDs in blood temperature downstream, and the compatible cardiac output computer computes a dilution curve via a modified Stewart-Hamilton indicator dilution equation.
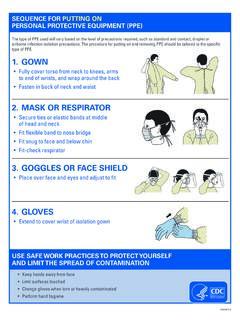
3 PA distal port Balloon inflation volume Pacing Preload Afterload Contractility Ventilation Pain Troubleshooting SQI for SVO2 Monitoring Transduce distal lumen CCO Swan-Ganz catheter Level Color Signal Description proper waveform is PA models require ml for inflation Level 1 Green Normal All aspects of the signal are optimal Level 2 Green Intermediate Indicates a moderately compromised signal Thermistor Level 3 Yellow Poor Indicates poor signal quality VIP port 4 cm from tip PEEP Muscle Level 4 Red Unacceptable Indicates severe problem with one or more aspects 30 cm from tip In main body of PA Activity of signal quality Located in RA/SVC Optimal RVEDVI SVR RVEF. Pulmonic valve R-R 60 100 mL/m2 800 1200 40 60% Signal quality may be compromised by: Proximal injectate port Thermal filament for CCO dyne-sec/cm-5. Pulsatility ( , wedging of catheter tip). 26 cm from tip 14-25 cm from tip Signal intensity ( , kinking of catheter, blood clot, hemodilution). Located in RA or SVC Rests between RA and RV Work of Breathing Intermittent wall contact by the catheter I f incorrectly positioned in S.
4 Hould be free floating and Optimal PAOP SVRI RVSWI. introducer sheath, bolus avoid endocardial surface P-R 6 12 mmHg 1970 2390 5 10 Signal quality may be improved by: CO measurement will be dyne-sec/ g-m/m2/beat E rroneous CCO Update entered hemoglobin and hematocrit values when there is a physiologic change erroneously high due to reflux cm-5/m2. measurement may result of 6% or greater in hematocrit or of g/dL ( mmol/L) or greater in hemoglobin of injectate within introducer if beyond pulmonic valve A. ttempt to distance electrocautery equipment and cables from the HemoSphere Advanced T. ransduce proximal injectate Tricuspid valve PADP PVR SVI Monitoring system lumen proper waveform is RA. 8 15 mmHg <250 33 47 Plug monitor cord into a separate AC circuit from the electrocautery equipment dyne-sec/cm-5 mL/beat/m2. CVP Troubleshooting CCO and CCOmbo catheters 2 6 mmHg Problem/. Applications and contraindications displayed message Possible cause Suggested action Clinical applications for Swan-Ganz Relative contraindications for Swan-Ganz CCO measurements I ncorrectly configured bolus V.
5 Erify that computation constant, Pulmonary artery catheters Pulmonary artery catheterization do not agree information injectate volume, and catheter size Acute heart failure There are no absolute contraindications Oxygen delivery Oxygen with bolus CO have been correctly selected F aulty thermistor or injectate DO2=CaO2 x CO x 10 Consumption measurements Severe hypovolemia to the use of a Pulmonary artery catheter; VO2=200-250 probe connection Use "iced" injectate and/or 10 mL injectate risk-benefit must be assessed for each patient 950 1150 mL/min mL/min volume to create a larger thermal signal Complex circulatory situations Unstable baseline temperature Things to consider before use include*: affecting bolus CO V. erify correct injection technique Medical emergencies Left bundle branch block measurements C. hange injectate temperature probe Acute respiratory distress syndrome Patients with tricuspid or pulmonic Gram negative sepsis Check thermal F low around thermal filament Flush catheter lumens heart valve replacements Drug intoxication filament position may be reduced Acute renal failure Presence of endocardial pacing leads Swan-Ganz catheter insertion waveforms T.
6 Hermal filament may be against V. erify proper catheter position in the Pulmonary artery: * Not an exhaustive list. Please see Hemorrhagic pancreatitis contraindications, precautions and vessel wall confirm wedge pressure balloon inflation Intra and post-operative management of high risk patients complications sections within the IFU. Right atrial/central venous Right ventricle volume C. atheter not in patient pressure (RA/CVP) S ystolic pressure (RVSP) of mL. History of Pulmonary or cardiac disease 2-6 mmHg 15-25 mmHg c onfirm appropriate catheter placement for Fluid shifts ( , extensive intra-abdominal operations) patient's height, weight, and insertion site Mean 4 mmHg D. iastolic pressure (RVDP). Management of high-risk obstetrical patients consider chest x-ray for evaluation of proper a = atrial systole 0-8 mmHg Diagnosed cardiac disease placement c=b ackward bulging from Toxemia Resume CO Monitoring tricuspid valve closure Premature separation of placenta v = a trial filling, ventricular systole Warm injectate I njectate temperature within Verify injectate fluid temperature Cardiac output determinations RA RV or injectate 8 C of blood temperature Use cooler injectate fluid: D.
7 Ifferential diagnosis of mitral regurgitation temperature I njectate temperature < 0 C, Maintain ice slush solution and ventricular septal rupture ECG ECG out of range, > 30 C, or > BT C. heck injectate probe connection Diagnosis of cardiac tamponade a c v a c v check probe I njectate temperature C. hange patient CCO cable RA RV probe malfunction R. eplace injectate temperature probe Catheter insertion distance markings SQI = 4 L ow blood flow at catheter tip Verify proper catheter position or catheter tip against vessel wall Update Hgb/Hct values using UPDATE function Location Distance to VC/RA Junction Distance to PA. S. ignificant change in Check catheter for kinking and recalibrate Internal jugular 15-20 cm 40-55 cm Pulmonary artery Pulmonary artery occlusion Hgb/Hct values Replace catheter if values required and recalibrate Subclavian vein 10-15 cm 35-50 cm S ystolic pressure pressure (PAOP) Catheter tip clotted Femoral vein 30 cm 60 cm (PASP) 15-25 mmHg Mean 6-12 mmHg A.
8 Fter all above troubleshooting measures are Catheter kinked or damaged utilized, press OPTICAL RESET. Right antecubital fossa 40 cm 75 cm a = atrial systole D. iastolic pressure Left antecubital fossa 50 cm 80 cm (PADP) 8-15 mmHg v = a trial filling, Note: Catheter markings occur every 10 cms and are denoted by a thin black line. 50 cm markings are denoted Red/IR transmit D. ebris or film obstructing C. lean oximetry cable / catheter connector M. ean pressure (MPA) ventricle systole by a thick black line. Catheter must exit introducer sheath before inflating balloon. 10-20 mmHg oximetry cable / catheter connectors with 70% isopropyl alcohol and connector lens swab, let air dry and recalibrate PA O. ximetry cable malfunction Power monitor off and on to restore platform PAOP. Parameters attained with ECG. Change oximetry cable and recalibrate ECG. HemoSphere Advanced Monitoring system a v a v PA. End-diastolic volume (EDV): The volume of blood in the ventricle at the end of the diastole.
9 PAW. EDV = SV/EF Thermal filament Normal RVEDV: 100 160 mL connector Thermistor Normal RVEDVI: 60 100 mL/m2 Proper Wedge Proper wedge Proper Wedge connector Ejection fraction (EF): The percentage of blood ejected from the ventricle with each beat. Optical module EF = _(EDV-ESV/EDV) x 100_ or EF = _SV/EDV x 100_ connector SvO2. Proximal EDV EDV injectate Volume infusion lumen hub Normal RVEF: 40 60%. Note: As with all measurements in Hemodynamic Monitoring , the absolute number is not as important as trends port (VIP) hub and changes in response to therapy. Appropriate a Over inflation Catheter too distal Catheter PA distal Stroke volume (SV): The volume of blood ejected from the ventricle in each beat and v waves of balloon Overdamping spontaneous wedging lumen hub SV = CO/HR x 1000 noted Note waveform rise of tracing Wedge type tracing Normal SV: 60 100 mL with balloon deflated Normal SVI: 33 47 mL/beat/m2 Balloon Note: As with all measurements in Hemodynamic Monitoring , the absolute number is not as important as trends inflation valve and changes in response to therapy.
10 Goal of RV volumetric measurements Volume Volume A. volume Volume Optimize RV efficiency 60 cm 70 cm 80 cm 90 cm 100 cm Stroke Stroke O. ptimize the relationship between EDV and SV. Stroke Stroke A. I n a volume responsive state, an increase in preload (EDV) End-Diastolic Volume End-Diastolic Volume End-Diastolic Volume End-diastolic volume will result in an increase in stroke volume (SV). Volume B. Prior to reaching the flat part of the curve, an increase in preload B. Volume volume Volume (EDV) will increase SV while not causing a decrease in ejection fraction Stroke 50 cm 40 cm 30 cm 20 cm Stroke Stroke C. On the flat part of the curve, a further increase in preload (EDV). Stroke Thermal will not result in an increase in SV End-Diastolic Volume End-Diastolic Volume 10 cm End-diastolic volume End-Diastolic Volume Filament C. Thermistor Volume volume At this point, a further increase in volume may: Volume Volume Decrease oxygen supply Stroke Stroke Stroke Stroke Increase oxygen demand End-Diastolic Volume End-diastolicVolume End-Diastolic volume Decrease left ventricular compliance End-Diastolic Volume Balloon Therapy should be directed at increasing contractility or reducing afterload.