Search results with tag "Explanation of benefits"
Understanding Your Explanation of Benefits
www.bcbstx.comAn Explanation of Benefits (EOB) is a notification provided to members when a health care benefits claim is processed by Blue Cross and Blue Shield of Texas (BCBSTX).
Understanding Coordination of Benefits (COB)
www.ab.bluecross.caWith COB, you submit claims to your benefits carrier first for adjudication and payment according to your coverage and benefits. Once you have received an Explanation of Benefits or statement from that benefits carrier, you can submit a claim for the eligible outstanding amount to your spouse’s plan or your second plan.
Reading your Explanation of Benefits - CMS
www.cms.gov$0.00 $0.00: $0.00 $2.15: $0.00 PDC: 2 3/20/14– ... Reading your Explanation of Benefits: Visit go.cms.gov/c2c for more information: CMS Product No. 11819: Paid for by the Department of Health & Human Services. Revised July 2018: Created Date: 7/24/2018 2:30:26 PM ...
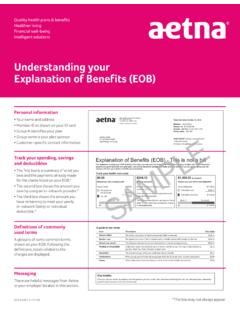
Understanding your Explanation of Benefits (EOB)
member.aetna.comOct 15, 2016 · Understanding your . Explanation of Benefits (EOB) Personal information • Your name and address • Member ID as shown on your ID card • Group # identifies your plan • Group name is your plan sponsor • Customer-specific contact information. Track your spending, savings and deductibles • The first box is a summary of what you
Table of Contents
padmin.comin mind you may need to submit appropriate documentation (e.g., Explanation of Benefits (EOB) or receipt(s)) to substantiate expenses. The NCFlex Convenience Card lets you pay a provider or vendor directly from your FSA at the point of purchase (if the provider accepts this form of …
NaviNet User Guide - content.highmarkprc.com
content.highmarkprc.comBenefits Submission If the member’s primary insurer is not Highmark, you will need to adjust the Coordination of Benefits for the claim. 1. Choose Claim Submission from the left navigation on Plan Central and then complete Patient Entry Screen. 2. Payer Screen: Fill in the primary payer Explanation of Benefits (EOB) information by changing ...
Enjoy the benefits - Aetna Dental
www.aetnadental.comdirectly into the account of your choice. It’s really that simple. Get our EFT enrollment form at joinaetnadentalnetwork.com. All the tools you need . Check claims status, access Explanation of Benefits (EOB) statements, get real-time eligibility and benefits data, and more — anytime, anywhere. With our tools, you can access
PROVIDER CLAIMS MANUAL
www.ilmeridian.comExplanation of Benefits (EOB) 23 Encounter Billing Guidelines – ERC, FQHC, and RHC 23 Electronic Claims Submission 23. Section . 6: Grievance and Appeals Process 2. 4 Grievance and Appeals Overview 24 Appeals 24 Member Expedited Appeals 25. Section . 7: Coordination of Benefits (COB) 27 Overview 27 Claims Guidelines for Dual-Eligible Members 27
National Drug Codes - UHCprovider.com
www.uhcprovider.comexplanation of benefits (EOB) or provider remittance advice (PRA) As a coordination of benefits (COB) claim (any primary payer; not limited to Medicare) COB submission The paper process2 (by fax), as noted in “How to submit NDC claims” Please submit both the CMS-1500 claim form and the primary carrier’s EOB together. NDC claim requirements
Practitioner and Provider Compliant and Appeal Request
www.aetna.comExplanation of Benefits (EOB) or other correspondence received from Aetna. Please provide the following information. (This information may be found on the front of the member’s ID card.) Today’s Date . Member’s ID Number . Plan Type . Medical . Dental . Member’s Group Number (Optional) Member’s First Name . Member’s Last Name .
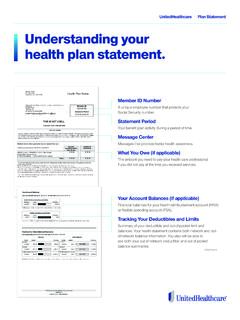
Unitedealthare lan tatement Understanding your health plan ...
www.myuhc.comUnderstanding your health plan statement. Please see the next page for more information ... The deductible is the fixed dollar amount that you pay each year toward eligible health care services before your plan benefits are payable. Once ... the Explanation of Benefits, or visit: www.myuhc.com. This is not a bill. Your provider will bill you ...
eBill Information and FAQs for Medical Providers
www.progressive.comexplanation of benefits (EOB) and payment? 1. After Progressive adjudicates the bill, AccidentEDI will send an 835 (eRemittance) to the original submitter of the related bill. The eRemittance serves as both the remittance advice and EOB. 2. Progressive will continue to send paper remittances and EOBs until further notice.
Claim EOB Tool: Access and Use - Aetna
www.aetna.comClaim EOB tool How to access and use the claim EOB tool Accessing the claim EOB tool The claim Explanation of Benefits (EOB) tool is available on our secure provider website on NaviNet®. The tool gives you access to EOBs available for taxpayer identification numbers (TINs). You can also view archived EOBs, back two years from the current date.
590154f Dental Claim Form Cigna
www.cigna.comWhen a claim is being submitted to the secondary payer, complete the entire form and attach the primary payer’s Explanation of Benefits (EOB) showing the amount paid by the primary payer. You may also note the primary carrier paid amount in the “Remarks” field (Item 35). There are additional detailed completion instructions in the CDT manual.
ANSI Denial Guide - CGS Medicare
www.cgsmedicare.comexplanation of benefits (EOB) information submitted with claim. The EOB information is required for Medicare to make a secondary payment. Determine if the patient has Group Health Plan coverage that is primary to Medicare. – If the patient has Group Health Plan coverage, resubmit the claim with the primary insurer’s EOB information.
Office manual for health care professionals - Aetna
www.aetnaeducation.comDispute submission Write to the PO box listed on the Explanation of Benefits (EOB) and/or the denial letter related to the issue you’re disputing.
Similar queries
Explanation of Benefits, Blue Cross and Blue Shield, Understanding, Of benefits, Your benefits, Your, Benefits, Reading, Understanding your Explanation of Benefits, Understanding your . Explanation of Benefits, Claim, S EOB, Aetna, Understanding your, Progressive, Cigna, CGS Medicare, Manual for health care professionals