Search results with tag "Authorization request"
Standardized Prior Authorization Request Form
www.commonwealthcarealliance.orgOct 14, 2021 · The standardized prior authorization form is intended to be used to submit prior authorizationrequests by Fax. Requesting providers should attach all pertinent medical documentation to support the request and submit to CCA for review. The Prior Authorization Request Form is for use with the following service types:
Prior Authorization Request Form–OUTPATIENT
www.cigna.comPrior Authorization Request Form–OUTPATIENT ... Note: In an effort to process your request in a timely manner, please submit any pertinent clinical information (i.e. progress notes, treatment rendered, test/lab results or radiology reports) to support the request for services. Any request for a non-contracted
ValueOptions Provider Guide to Online Authorization Requests
www.valueoptions.comGuide to Online Authorization Requests 4/9/2012 Page 6 Authorization Request for Continuing Care If there is a current authorization for the client, the user may be prompted to confirm that
Provider Preauthorization and Precertification Requirements
www.bcbsm.com• E-referral Electronic system for Michigan providers to submit requests for inpatient admission. ... Note: If you fail to submit your authorization request, submit an untimely request or your request is ... • Commercial PPO LTAC/SNF Enhancement Form Providers can call 1-800-249-5103 to obtain a status on Precertification requests by ...
C-4 ATTENDING DOCTOR'S REQUEST FOR AUTHORIZATION
thedisabilityguys.comAUTHORIZATION REQUEST First MI Last Number and Street City State Zip CodeNumber and Street City State Zip CodeC-4AUTH (12-14) Page 1 of 2The undersigned requests written authorization for the following www.wcb.ny.gov special service(s) costing over $1,000 or requiring pre-authorization pursuant to the Medical Treatment Guidelines. Do
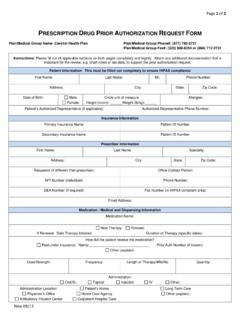
PRESCRIPTION D PRIOR AUTHORIZATION REQUEST FORM
www.care1st.comPage 2 of 2 New 08/13 PRESCRIPTION DRUG PRIOR AUTHORIZATION REQUEST FORM Patient Name: ID#: Instructions: Please fill out all applicable sections on both pages completely and legibly.Attach any additional documentation that is important for the review, e.g. chart notes or lab data, to support the prior authorization request.
Texas Standard Prior Authorization Request Form for Health ...
www.bcbstx.comTitle: Texas Standard Prior Authorization Request Form for Health Care Services Author: Texas Department of Insurance Keywords: prior authorization request form, NOFR001, SB 1216
Introducing: Standardized Prior Authorization Request Form
healthplansinc.comauthorization request forms (including all pertinent medical documentation) for submission to the appropriate health plan ... physician as the requesting provider or the facility where the service will be provided. † The contact person is the person who is filling out the form.
AltaMed Authorization Request Form
www.altamed.orgALTAMED AUTHORIZATION REQUEST FORM URGENT (72 HOURS) Requests submitted as an urgent referral when standard timeframes could seriously jeopardize the Member's life or health or ability to attain, maintain or regain maximum function.
2019 Aranesp (darbepoetin alfa) Prior Authorization Request
www.aetna.com2019 Aranesp® (darbepoetin alfa) Prior Authorization Request Page 1 of 3 (You must complete all 3 pages.) Fax completed form to: 1-800-408-2386 . For urgent requests, please call: 1-800-414-2386
Services that require authorization for Michigan providers
ereferrals.bcbsm.comrehabilitation, skilled nursing facility and long-term acute care hospital) See “Post-acute care services (long-term acute care, skilled nursing and rehabilitation facilities).” Left atrial appendage closure . Prior authorization is required. Use the e-referral system to submit the request and ... Look in the "Submit authorization request
Electroconvulsive Therapy (ECT) Authorization Request Form
www.coordinatedcarehealth.comELECTROCONVULSIVE THERAPY (ECT) Authorization Request Form *All Fields Must Be Completed For This Request To Be Reviewed. Please type or print neatly. Please indicate which level of care the member is currently engaged: INPATIENT OUTPATIENT . DEMOGRAPHICS . Patient Name . Patient Last Name . DOB . SSN .
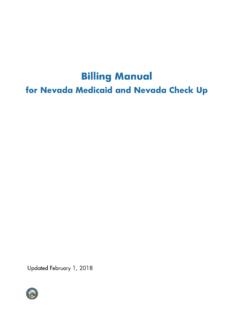
NV Billing General - Nevada Medicaid
www.medicaid.nv.govUpdated 02/01/2018 Billing Manual pv01/08/2018 v Ways to request authorization Drug requests and ProDUR overrides Submission deadlines Continued stay request
Introducing: Standardized Prior Authorization Request Form
www.hcasma.orgMassachusetts Administrative Simplification Collaborative–Standardized Prior Authorization Request Form V1.1 May 2012
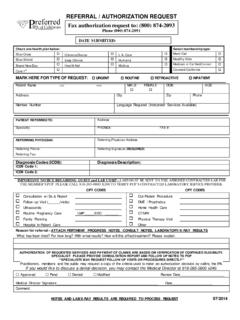
Phone (800) 874 -2091 DATE SUBMITTED:
www.preferredipa.comFax authorization request to: (800) 874-2093 Phone (800) 874 -2091 REFERRAL / AUTHORIZATION REQUEST . Check one health plan below: Select membership type:
Durable Medical Equipment (DME) Authorization Request
www.bcbst.comDurable Medical Equipment (DME) Authorization Request Please type/print legibly and fax completed form to: Commercial Utilization Management at 1-866-558-0789 OR
Prior Authorization Request (PAR) Coversheet
www.cgsmedicare.comTitle: Prior Authorization Request \(PAR\) Coversheet \(DME MAC Jurisdiction C\) Author: CGS - CH Subject: DME MAC JC Created Date: 1/2/2018 2:09:12 PM
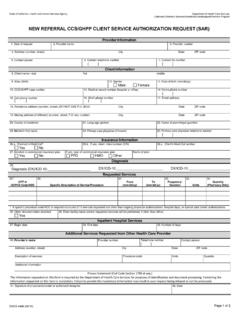
New Referral CCS/GHPP Client Service Authorization …
www.dhcs.ca.govNEW REFERRAL CCS/GHPP CLIENT SERVICE AUTHORIZATION REQUEST (SAR) Provider Information. 1. Date of request 2. Provider name 3. Provider number 4. Address (number, street) City State ZIP code . 5. Contact person 6. Contact telephone number ( ) 7. Contact fax number ( ) Client Information. 8. Client name—last first middle . 9. Alias (AKA) 10. Gender
Durable Medical Equipment (DME) Authorization Request
www.bcbst.comDurable Medical Equipment (DME) Authorization Request Please type/print legibly and fax completed form to: Commercial Utilization Management at 1-866-558-0789 OR
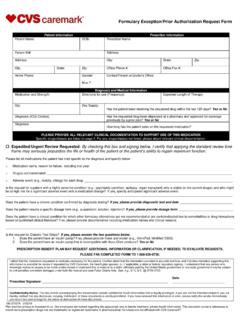
Formulary Exception/Prior Authorization Request Form
www.caremark.com5. Is the request for sumatriptan injection, sumatriptan nasal spray, or zolmitriptan nasal spray for cluster headache, and if the requested drug will be used concurrently with another triptan, the patient requires more than one triptan due to clinical need for …
DRUG FORMULARY
www.wcb.ny.govA Prior Authorization request that is not responded to within four calendar days (by an approval, denial or partial approval) may be deemed approved as prescribed, not to exceed a 365-day supply, upon issuance of an Order of the Chair. (3) A partial approval or denial of a Prior Authorization request must: a.
MEDICARE ADVANTAGE AUTHORIZATION REQUIREMENTS
medicareproviders.cigna.comAn authorization number or referral number is not a guarantee of payment. Please always verify benefits. Authorization requests can be submitted by phone, fax or via web-based HS Connect (HSC) (HS Connect not currently available for Arizona and Leon). For an overview of capabilities and instructions for obtaining access, visit the HSC
Nonemegency Ambulance Prior Authorization …
www.tmhp.comTexas Medicaid and Children with Special Health Care Needs (CSHCN) Services Program Non-emergency Ambulance Prior Authorization Request Submit completed form by fax to: 1-512-514-4205
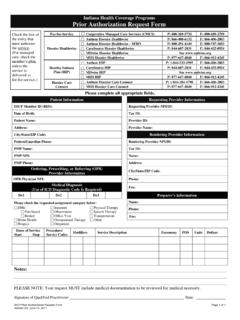
Indiana Health Coverage Programs Prior Authorization ...
www.mdwise.orgIHCP Prior Authorization Request Form Page 1 of 1
Repetitive, Scheduled Non-Emergent Ambulance Transport ...
www.cms.govDec 01, 2015 · Prior authorization is voluntary; however, if the ambulance supplier elects not to submit a prior authorization request before the fourth round trip in a 30-day period, the claim related to the repetitive, scheduled non-emergent ambulance transport will be subject to a prepayment medical record review. 3.1 - Model Inclusion
DENTAL PRIOR APPROVAL AUTHORIZATION …
www.michigan.govPage 1 of 2 MSA-1680-B (Rev. 10/16) Previous Editions Obsolete MICHIGAN DEPARTMENT OF HEALTH AND HUMAN SERVICES . DENTAL PRIOR APPROVAL AUTHORIZATION REQUEST . Instructions for MSA-1680-B
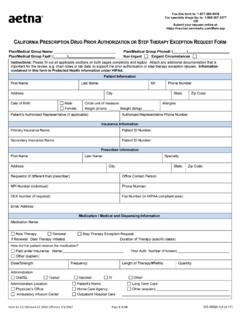
Prescription Drug Prior Authorization Request Form - Aetna
www.aetna.comForm 61-211 (Revised 12-2016) Effective 7/1/2017 Page 3 of 10 GR-69025-CA (5-17) Aetna complies with applicable Federal civil rights laws and does not discriminate, exclude or treat
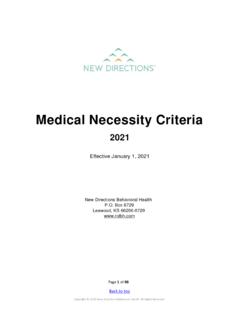
Medical Necessity Criteria - BCBSM
www.bcbsm.comElectroconvulsive Therapy (ECT): Inpatient Criteria..... 68 Electroconvulsive Therapy (ECT): Outpatient Criteria..... 70 23- Hour Observation Criteria ... The Continued Authorization Request(s) section details the documented present symptoms, behaviors, or functional impairments exhibited by the member at the time of the concurrent ...
PLEASE READ CAREFULLY THE FOLLOWING INFORMATION …
www.wcb.ny.govThe self-insured employer/insurer must respond to the authorization request orally and in writing via email, fax or regular mail with confirmation of delivery within 30 days. The 30 day time period for response begins to run from the completion date of this form if emailed or faxed, or the completion date plus five days if sent via regular mail.
Medical Exception/ Fax this form to: 1-877-269-9916 OR ...
www.aetna.comThis pre-authorization request form should be filled out by the provider. Before completing this form, please confirm the patient’s benefits and eligibility.
Similar queries
Authorization request, AUTHORIZATION, Request, ValueOptions Provider Guide to Online Authorization Requests, Guide to Online Authorization Requests, Referral, Commercial, Form, Special, PRESCRIPTION D PRIOR AUTHORIZATION REQUEST FORM, PRIOR AUTHORIZATION REQUEST FORM, Texas Standard Prior Authorization Request Form, Prior Authorization Request, Service, Rehabilitation, Skilled nursing facility, Skilled nursing, ELECTROCONVULSIVE THERAPY (ECT) Authorization Request, NV Billing General, Nevada, Request authorization, Introducing: Standardized Prior Authorization Request, 800) 874 -2091 DATE SUBMITTED, REFERRAL / AUTHORIZATION REQUEST, Durable Medical Equipment (DME) Authorization Request, Drug, DRUG FORMULARY, Authorization requests, Texas Medicaid and Children with Special, Health Coverage Programs Prior Authorization, Repetitive, scheduled non-emergent ambulance transport, PRIOR, Aetna, Electroconvulsive Therapy, Confirmation, Exception