Medicaid Provider Enrollment Requirements by State
have prior authorization. No Requirements: For services other than emergency that require prior authorization, the out-of-state provider must confirm, in writing, that he or she will enroll in the South Carolina Medicaid program and will accept Medicaid reimbursement as payment in full. Reference to Requirements: Provider Enrollment Information
Tags:
States, Requirements, Medicaid, Provider, Authorization, Enrollment, Prior, Prior authorization, Medicaid provider enrollment requirements by state
Information
Domain:
Source:
Link to this page:
Please notify us if you found a problem with this document:
Documents from same domain
Some authorization requirements vary by member plan. s ...
content.highmarkprc.comstanding frame/table system, one position (e.g., upright, supine or prone stander), any size including pediatric, with or without wheels e0639 patient lift, moveable from room to room with disassembly and reassembly, includes all components/accessories e0642 standing frame/table system, mobile (dynamic stander), any size including pediatric
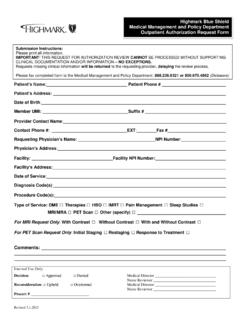
Highmark Blue Shield Medical Management and …
content.highmarkprc.comRevised 3.1.2015 Name of Requestor/Contact Person: _____ Patient’s Name: Patient Phone # Patient’s Address: Date of Birth: Member UMI: Suffix # …
Highmark Blue Shield Medical Management and Policy ...
content.highmarkprc.com3.1.2016 CLINICAL DOCUMENTATION AND Name of Requestor/Contact Person Requestor’s Phone Number Member ID Number Patient Name Patient Phone Number
Policy, Medical, Blue, Shield, Highmark, Highmark blue shield medical
Advanced Imaging and Cardiology Services Program Codes ...
content.highmarkprc.com75565 Cardiac magnetic resonance imaging for velocity flow mapping (list separately in addition to code for primary procedure) 75571 . Computed tomography, heart, without contrast material, with …
NaviNet User Guide - content.highmarkprc.com
content.highmarkprc.comBenefits Submission If the member’s primary insurer is not Highmark, you will need to adjust the Coordination of Benefits for the claim. 1. Choose Claim Submission from the left navigation on Plan Central and then complete Patient Entry Screen. 2. Payer Screen: Fill in the primary payer Explanation of Benefits (EOB) information by changing ...
Benefits, Claim, Explanation, Explanation of benefits, Of benefits
SPECIALTY DRUG REQUEST FORM
content.highmarkprc.comSPECIALTY DRUG REQUEST FORM To view our formularies on-line, please visit our Web site at the addresses listed above. Fax each form separately. Please use a separate form for each drug.Print, type or write legibly in blue or black ink. See reverse side for additional details. Once completed, please fax this form to1-866-240-8123.
2021 Adult Preventive Health Guidelines: Ages 19 through ...
content.highmarkprc.comThe USPSTF recommends against screening for cervical cancer in women who have had a hysterectomy with removal of the cervix and do not have a history of a high-grade precancerous lesion (ie, cervical intraepithelial neoplasia [CIN] grade 2 or 3) or cervical cancer.D Recommendation
Highmark Reimbursement Policy Bulletin
content.highmarkprc.comJul 15, 2019 · Page 3 of 12 When a covered benefit, evaluation and management and consultation services delivered through telehealth for *new and established patients may be reimbursed under the following conditions: *Note: In accordance with the telehealth waiver issued by CMS related to the 2019 novel coronavirus, new patients will be permitted to receive telehealth services …
F02 General Consent For Medical/Surgical Procedures ...
content.highmarkprc.comGeneral Consent For Medical/Surgical Procedures/Interventions _____ _____ Patient Name Medical Record Number TO THE MEMBER: You have been given information about your condition and the recommended surgical, medical, or diagnostic procedure(s). This consent form is designed to provide a written ...
Physician Patient Termination Letter
content.highmarkprc.comTHIS IS ONLY A SAMPLE!!! PLEASE WRITE YOUR OWN BASED ON THE SPECIFIC NEEDS/SITUATION OF YOUR PRACTICE. PHYSICIAN/PATIENT TERMINATION PROTOCOLS The patient must be given clear and reasonable notice of the physician’s intent to withdraw as the primary care physician from the case. If at all possible, the
Patients, Your, Practices, Samples, This, Only, Your practice, This is only a sample
Related documents
PHC TAR REQUIREMENTS - partnershiphp.org
www.partnershiphp.org[Treatment Authorization Request (TAR) to be submitted by the provider performing these services] Page 1 of 7 PHC TAR REQUIREMENTS A. Acupuncture (see policy MCUG3002 Acupuncture Service Guidelines) A RAF is required for the first visit, and then members are limited to 2 visits per month. A TAR is required if services exceed two visits per month.
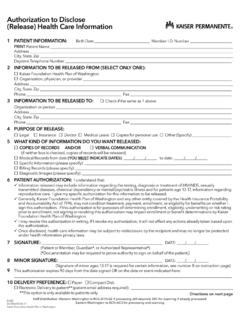
Authorization for Use or Disclosure of Patient Health ...
wa.kaiserpermanente.orgon whether I sign this authorization. If this authorization is for purposes of determining enrollment, eligibility, underwriting or risk rating prior to enrollment, not signing or revoking this authorization may impact enrollment or benefit determinations by …