Transcription of CHAPTER 1: OPINIONS ON PATIENT-PHYSICIAN …
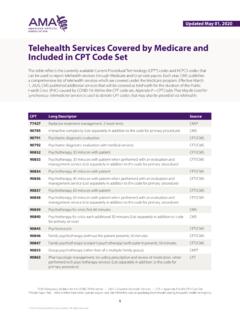
1 CHAPTER 1: OPINIONS ON PATIENT-PHYSICIAN RELATIONSHIPS The OPINIONS in this CHAPTER are offered as ethics guidance for physicians and are not intended to establish standards of clinical practice or rules of law. Responsibilities of Physicians & Patients PATIENT-PHYSICIAN Relationships Prospective Patients Patient Rights Patient Responsibilities Terminating a PATIENT-PHYSICIAN Relationship Quality Physician Exercise of Conscience Physician Responsibilities for Safe Patient Discharge from Health Care Facilities Special Issues in PATIENT-PHYSICIAN Relationships Treating Self or Family Discrimination and Disruptive Behavior by Patients Consultation, Referral & Second OPINIONS Use of Chaperones Sports Medicine Work-Related & Independent Medical Examinations Use of Restraints Gifts from Patients Use of Remote Sensing & Monitoring Devices Political Action by Physicians Ethically Sound Innovation in Medical Practice Ethical Practice in Telemedicine Medical Tourism PATIENT-PHYSICIAN Relationships The practice of medicine, and its embodiment in the clinical encounter between a patient and a physician.
2 Is fundamentally a moral activity that arises from the imperative to care for patients and to alleviate suffering. The relationship between a patient and a physician is based on trust, which gives rise to physicians ethical responsibility to place patients welfare above the physician s own self-interest or obligations to others, to use sound medical judgment on patients behalf, and to advocate for their patients welfare. A PATIENT-PHYSICIAN relationship exists when a physician serves a patient s medical needs. Generally, the relationship is entered into by mutual consent between physician and patient (or surrogate). However, in certain circumstances a limited PATIENT-PHYSICIAN relationship may be created without the patient s (or surrogate s) explicit agreement. Such circumstances include: (a) When a physician provides emergency care or provides care at the request of the patient s treating physician. In these circumstances, the patient s (or surrogate s) agreement to the relationship is implicit.
3 (b) When a physician provides medically appropriate care for a prisoner under court order, in keeping with ethics guidance on court-initiated treatment. (c) When a physician examines a patient in the context of an independent medical examination, in keeping with ethics guidance. In such situations, a limited PATIENT-PHYSICIAN relationship exists. AMA Principles of Medical Ethics: I,II,IV,VIII Prospective Patients As professionals dedicated to protecting the well-being of patients, physicians have an ethical obligation to provide care in cases of medical emergency. Physicians must also uphold ethical responsibilities not to discriminate against a prospective patient on the basis of race, gender, sexual orientation or gender identity, or other personal or social characteristics that are not clinically relevant to the individual s care. Nor may physicians decline a patient based solely on the individual s infectious disease status. Physicians should not decline patients for whom they have accepted a contractual obligation to provide care.
4 However, physicians are not ethically required to accept all prospective patients. Physicians should be thoughtful in exercising their right to choose whom to serve. A physician may decline to establish a PATIENT-PHYSICIAN relationship with a prospective patient, or provide specific care to an existing patient, in certain limited circumstances: (a) The patient requests care that is beyond the physician s competence or scope of practice; is known to be scientifically invalid, has no medical indication, or cannot reasonably be expected to achieve the intended clinical benefit; or is incompatible with the physician s deeply held personal, religious, or moral beliefs in keeping with ethics guidance on exercise of conscience. (b) The physician lacks the resources needed to provide safe, competent, respectful care for the individual. Physicians may not decline to accept a patient for reasons that would constitute discrimination against a class or category of patients (c) Meeting the medical needs of the prospective patient could seriously compromise the physician s ability to provide the care needed by his or her other patients.
5 The greater the prospective patient s medical need, however, the stronger is the physician s obligation to provide care, in keeping with the professional obligation to promote access to care. (d) The individual is abusive or threatens the physician, staff, or other patients, unless the physician is legally required to provide emergency medical care. Physicians should be aware of the possibility that an underlying medical condition may contribute to this behavior. AMA Principles of Medical Ethics: I,VI,VIII,X Patient Rights The health and well-being of patients depends on a collaborative effort between patient and physician in a mutually respectful alliance. Patients contribute to this alliance when they fulfill responsibilities they have, to seek care and to be candid with their physicians. Physicians can best contribute to a mutually respectful alliance with patients by serving as their patients advocates and by respecting patients rights. These include the right: (a) To courtesy, respect, dignity, and timely, responsive attention to his or her needs.
6 (b) To receive information from their physicians and to have opportunity to discuss the benefits, risks, and costs of appropriate treatment alternatives, including the risks, benefits and costs of forgoing treatment. Patients should be able to expect that their physicians will provide guidance about what they consider the optimal course of action for the patient based on the physician s objective professional judgment. (c) To ask questions about their health status or recommended treatment when they do not fully understand what has been described and to have their questions answered. (d) To make decisions about the care the physician recommends and to have those decisions respected. A patient who has decision-making capacity may accept or refuse any recommended medical intervention. (e) To have the physician and other staff respect the patient s privacy and confidentiality. (f) To obtain copies or summaries of their medical records. (g) To obtain a second opinion.
7 (h) To be advised of any conflicts of interest their physician may have in respect to their care. (i) To continuity of care. Patients should be able to expect that their physician will cooperate in coordinating medically indicated care with other health care professionals, and that the physician will not discontinue treating them when further treatment is medically indicated without giving them sufficient notice and reasonable assistance in making alternative arrangements for care. AMA Principles of Medical Ethics: I,IV,V,VIII,IX Patient Responsibilities Successful medical care requires ongoing collaboration between patients and physicians. Their partnership requires both individuals to take an active role in the healing process. Autonomous, competent patients control the decisions that direct their health care. With that exercise of self-governance and choice comes a number of responsibilities. Patients contribute to the collaborative effort when they: (a) Are truthful and forthcoming with their physicians and strive to express their concerns clearly.
8 Physicians likewise should encourage patients to raise questions or concerns. (b) Provide as complete a medical history as they can, including providing information about past ill nesses, medications, hospitalizations, family history of illness, and other matters relating to present health. (c) Cooperate with agreed-on treatment plans. Since adhering to treatment is often essential to public and individual safety, patients should disclose whether they have or have not followed the agreed-on plan and indicate when they would like to reconsider the plan. (d) Accept care from medical students, residents, and other trainees under appropriate supervision. Participation in medical education is to the mutual benefit of patients and the health care system; nonetheless, patients (or surrogates ) refusal of care by a trainee should be respected in keeping with ethics guidance. (e) Meet their financial responsibilities with regard to medical care or discuss financial hardships with their physicians.
9 Patients should be aware of costs associated with using a limited resource like health care and try to use medical resources judiciously. (f) Recognize that a healthy lifestyle can often prevent or mitigate illness and take responsibility to follow preventive measures and adopt health-enhancing behaviors. (g) Be aware of and refrain from behavior that unreasonably places the health of others at risk. They should ask about what they can do to prevent transmission of infectious disease. (h) Refrain from being disruptive in the clinical setting. (i) Not knowingly initiate or participate in medical fraud. (j) Report illegal or unethical behavior by physicians or other health care professionals to the appropriate medical societies, licensing boards, or law enforcement authorities. AMA Principles of Medical Ethics: I,IV,VI Terminating a PATIENT-PHYSICIAN Relationship Physicians fiduciary responsibility to patients entails an obligation to support continuity of care for their patients.
10 At the beginning of PATIENT-PHYSICIAN relationship, the physician should alert the patient to any foreseeable impediments to continuity of care. When considering withdrawing from a case, physicians must: (a) Notify the patient (or authorized decision maker) long enough in advance to permit the patient to secure another physician. (b) Facilitate transfer of care when appropriate. AMA Principles of Medical Ethics: I,VI Quality As professionals dedicated to promoting the well-being of patients, physicians individually and collectively share the obligation to ensure that the care patients receive is safe, effective, patient centered, timely, efficient, and equitable. While responsibility for quality of care does not rest solely with physicians, their role is essential. Individually and collectively, physicians should actively engage in efforts to improve the quality of health care by: (a) Keeping current with best care practices and maintaining professional competence.